Part 16 in our LTC Seating & Positioning series intended to shed some light on the mystery of seating and positioning in the LTC setting. See the rest of the blog posts in the following links: Part 1 (Best Wheelchair Options in LTC), Part 2 (Posture Problems), Part 3 (Posterior Pelvic Tilt), Part 4 (Anterior Pelvic Tilt), Part 5 (Pelvic Obliquity), Part 6 (Pelvic Rotation), Part 7 (Fixed vs Flexible Postural Abnormalities), Part 8 (Windswept Posture), Part 9 (Incorrect Seating Dimensions), Part 10 (Issues with Current Wheelchair System: Seat-to-Floor-Height), Part 11 (Issues with Current Wheelchair System: Back Support), Part 12 (Issues with Current Wheelchair System: Legrest), Part 13 (Issues with Current Wheelchair System: Armrest), Part 14 (Issues with Current Wheelchair System: Head Support), Part 15 (Why is wheelchair seating & positioning important for our residents?)
One of the questions that comes up in regards to doing a seating evaluation is: how is a seating evaluation different than a typical OT/PT eval? Don't let the term "Seating Evaluation" scare you! The following lists are some guidelines to conducting a successful seating evaluation.
Guideline for a Successful Seating Evaluation
- Conduct your evaluation as you would any other OT/PT eval in the nursing home to determine functional needs of the resident
- Assess limitations in ROM, strength, balance, and endurance and how they negatively affect posture in the wheelchair
- Is there a postural abnormality? Decide if that postural abnormality is flexible or fixed: should your goal be to correct or accommodate for it?
- Choose an appropriate wheelchair model that allows for adjustability, seat cushion, back support, head support, and accessories to address the resident's physical limitations.
- Use the measurements form provided to take key measurements.
- Match the wheelchair size to the resident's dimensions to ensure a proper fit.
*Don't forget to look for hip contractures and tight hamstrings during the evaluation. They are often the culprits of poor pelvic positioning!
Measuring Guide
Here is an easy to use measurement form with the measurements included in an LTC seating and positioning evaluation along with some tips to review to make sure your seating evaluation is successful. There will also be a pdf to follow for you to print out and take along for LTC seating and positioning evaluations. Before we get to the measuring guide here are a few tips to review to make sure your seating evaulation is successful.
Measuring Tips
- All measurements should be taken while sitting on a firm, flat surface in the posture the therapist is trying to accomplish for the resident.
- Measure using a hard measuring tape, not one that can bend and wrap around the patient's body. That will lead to measurement errors, adding circumference or length.
- All measurements should be taken straight across the body.
- Use a measurement form to remind you of the measurements needed to be taken and to record them properly.
Measuring Guide
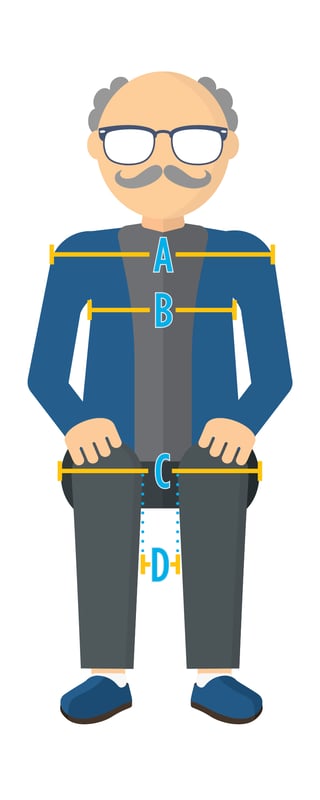 |
A - Shoulder Width |
|
B - Chest Width |
|
| C - Hip Width | |
| D - Between Knees | |
| *Don't forget to inclued excess tissue in all measurements and measure the resident in their ideal posture |
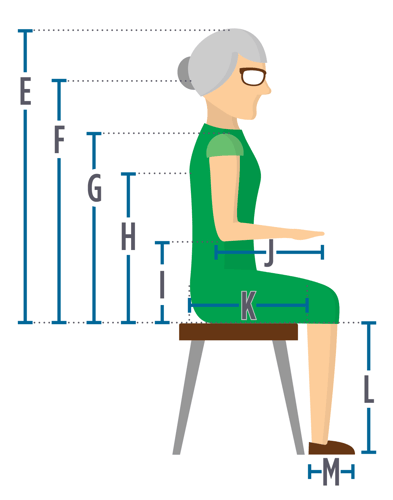 |
E - Top of Head |
|
F - Occiput |
|
|
G - Seat to Top of Shoulder |
|
|
H - Inferior Angle of Scapula |
|
|
I - Seat to Elbow |
|
|
J - Lower Arm Length |
|
|
K - Upper Leg Length |
|
|
L - Lower Leg Length |
|
|
M - Foot Length |
If time is a constraint, the four measurements you MUST do are:
- Hip Width (C)
- Seat to Top of Shoulder (G)
- Upper Leg Length (K)
- Lower Leg Length (L)
These will allow you to match a wheelchair, including a cushion and back support, to your resident.
Check back next week when we break down how to measure specifically for seat dimensions, seat-to-floor-height, back support, leg rests, armrest, and head support.

Ana Endsjo, MOTR/L, CLT
Clinical Education Manager LTC Division
Ana Endsjo has worked as an occupational therapist since 2001 in a variety of treatment settings. She has mainly worked with the geriatric population, dedicated to the betterment of the treatment of the elderly in LTC centers. Her focus has been on seating and positioning and contracture management of the nursing home resident. With this experience, her hope is to guide other therapists, rehab directors, nurses, and administrators through educational guides, blogs, webinars, and live courses in her role as Clinical Education Manager for the long term care division.