Part 3 in our LTC Seating & Positioning series is intended to shed some light on the mystery of seating and positioning in the LTC setting. See Part 1 and Part 2. Check out a digital rehab version of the LTC Seating & Positioning Guide here.
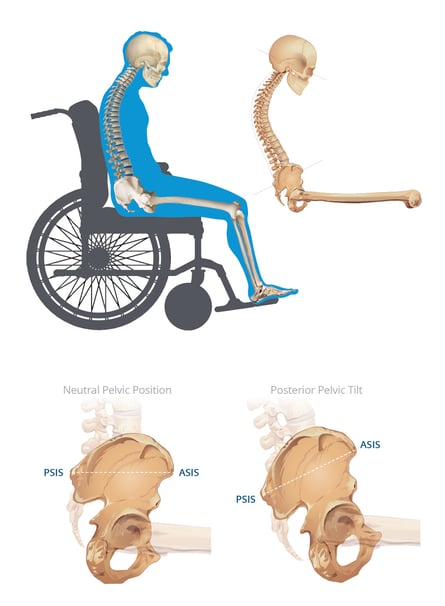
Posterior pelvic tilt is probably the most commonly seen postural abnormality, and many of us know it better as the dreaded sacral sitting position! We call it sacral sitting because the pelvis is tilted in such a way that all the pressure is placed directly on the sacrum, leaving our residents highly susceptible to a pressure injury.
Let's review the causes of posterior pelvic tilt and how our residents end up in a sacral sitting position:
|
What is the pelvis doing? |
ASIS is higher than the PSIS resulting in the posterior pelvic tilt/sacral sitting posture |
|
What is the spine doing? |
Excessive thoracic kyphosis producing the "C" shape spine Lordosis curvature of the lumbar and cervical spine "flatten out" |
|
What are the head and neck doing? |
Excessive forward neck flexion Eye gaze to the lap or the floor |
Why is the Sacral Sitting posture so dangerous to our elderly residents?
The excessive “C” curvature causes chest and abdominal constriction. The organs housed in the chest and abdomen are unable to function properly, placing an immune-compromised elderly resident even more at risk for infection and system failure.
Chest constriction produces complications:
- Inadequate inflation of lungs and diaphragm
- Residents take more shallow, quicker breaths for respiration
- Quicker breaths expend more energy, causing fatigue when trying to sit up against gravity and for the system to function properly
- Fluid pools in the lungs and increases the risk of pneumonia
Abdominal constriction places pressure on the digestive tract and bladder, causing:
- Increased risk of constipation and bowel impaction
- Gastritis and reflux issues
- Inadequate emptying of the bladder leading to an increased risk of UTIs, bladder, and kidney infection
The head and neck can also be significantly affected with a posterior pelvic tilt and an excessive kyphosis. The neck can go into excessive forward flexion with the head pointed straight down to the lap or floor. Often the chin is “buried” in the resident’s chest. This can negatively impact various areas of function for the resident. The unnatural head position can lead to swallowing difficulties and an increased susceptibility for:
- Choking
- Aspiration
Visual field and ability to communicate can also be impacted with this unnatural head position:
- Eye gaze is no longer in midline but straight downward, and the resident often lacks the neck strength to bring the head up against gravity
- Residents can’t lift head to midline to see whom they are speaking to and have a tendency to withdraw from others and activities
- Fatigue and inadequate breath produce poor voice projection and quality
So, what should the therapist aim for when a posterior pelvic tilt has been identified?
- Avoid the use of elevating leg rests that shorten hamstrings length, creating a pull on the pelvis into a posterior pelvic tilt.
- If the posterior pelvic tilt symptoms are flexible, try an anti-thrust component to reduce forward migration of the pelvis into sacral sitting.
- Ensure appropriate cushion depth to prevent contact pressure behind the knees. Pressure behind the knees promotes the likelihood of the resident sliding forward to alleviate discomfort or decreased LE circulation.
- Look for a wheelchair model or a back support that can open seat-to-back angle to straighten out the chest and place the pelvis at an angle the resident can tolerate. This will prevent unwanted forward migration of the pelvis.
- Use a cushion with medial and lateral contour to promote LE alignment and pelvic stability. The medial abductors and lateral adductors will form leg troughs to help align the LEs and pelvis in a midline posture.
- Add a solid seat insert to any seat sling that is hammocking to prevent the pelvis from collapsing into a posterior pelvic tilt.
- If the posterior pelvic tilt symptoms are flexible, load the trochanters with a cushion with tapered lateral adductors to stabilize the pelvis in the resident’s most neutral alignment.
- If it is a fixed posterior pelvic tilt, use an immersion style cushion that contours to the shape of the resident for maximum pressure redistribution, minimizing peak pressures.
- ELRs also decrease femoral contact with the seat surface, increasing the posterior pelvic tilt posture and placing a downward pressure on the bony prominences. The increased pressure at the ITs, sacrum, and coccyx increase the risk of a pressure injury.
By understanding this commonly seen abnormal posture, you will identify the posterior pelvic tilt causes more easily when performing your screens and evaluations. Understanding what you are up against will guide your choices in selecting wheelchair seat cushions, back supports, and accessories to optimize the seating system to fit the individualized need of every resident.

Ana Endsjo, MOTR/L, CLT
Clinical Education Manager LTC Division
Ana Endsjo has worked as an occupational therapist since 2001 in a variety of treatment settings. She has mainly worked with the geriatric population, dedicated to the betterment of the treatment of the elderly in LTC centers. Her focus has been on seating and positioning and contracture management of the nursing home resident. With this experience, her hope is to guide other therapists, rehab directors, nurses, and administrators through educational guides, blogs, webinars, and live courses in her role as Clinical Education Manager for the long term care division.