Part 5 in our LTC Seating & Positioning series intended to shed some light on the mystery of seating and positioning in the LTC setting. See Part 1, Part 2, Part 3, and Part 4. Check out our digital, rehab-focused Wheelchair Seating & Positioning Guide here.
A pelvic obliquity is a very common abnormality in the nursing home. Less common is the knowledge that, more times than not, the obliquity is caused by the resident’s wheelchair system.
I know firsthand that ordering a new wheelchair for every resident is unlikely. We must use the wheelchair model available in the storage closet whether or not it is the correct size to match the resident’s dimensions. This ill-fitting wheelchair can be to blame for a resident’s abnormal posture.
The ill-fitting wheelchair may be to blame for pelvic obliquity when:
- The seat sling is hammocking
- Seat width is too wide
- Back support height is too low
- Only one leg rest is being used
- Foot plates are set at unequal heights
- Armrest height is too high or too low
Whether the reason is the ill-fitting wheelchair or an anatomical issue with the resident or a combination of the two, how do you identify an obliquity?
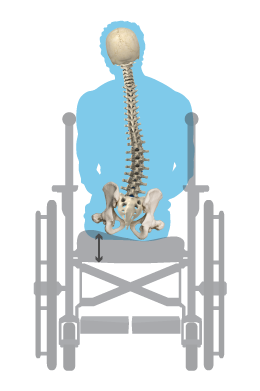
Let's check out what is going on at the pelvis, spine, head, and neck to be able to quickly identify the issue by sight:
|
|
|
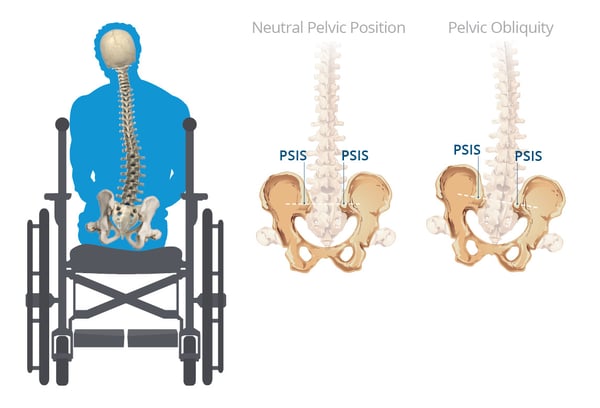
What is the pelvis doing?
|
Pelvis sits with the L or R ASIS higher than the other, causing the raising up of one hip.
|
|
What is the spine doing?
|
When one side of the pelvis is raised higher than the other, our body’s natural righting reactions attempt to bring the spine back to midline. The thoracic spine on the lower side curves back towards the midline, creating a scoliosis over time. Most residents lack the strength to bring the trunk back to midline, so you are presented with a laterally-leaning trunk with a scoliotic spine.
|
|
What are the head and neck doing?
|
The neck will go into lateral flexion as if the person is dropping the ear to his or her shoulder.
|
What should our wheelchair positioning goals be when presented with a resident with a pelvic obliquity?
The answer to that question depends on whether the abnormality is fixed or flexible. Remember, when a pelvic abnormality is flexible, you will be able to move the pelvis out of the posture and back to a neutral pelvis. If your goal is to correct the abnormality:
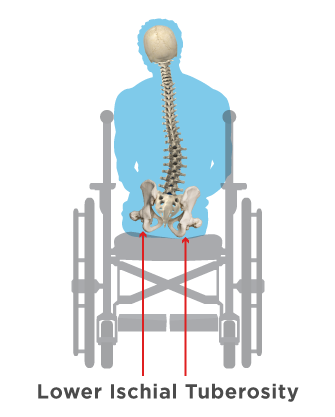
- Attempt to level the pelvis by building up the lower IT with an adjustable cushion.
- Remember you may have to incrementally build up the lower side to allow the resident time to adjust to the changes and tolerate the change without pain or discomfort.
If the pelvis obliquity is fixed, the primary need is for even pressure distribution to take excess pressure off the lower IT, protecting it from wound development. Additional goals with a fixed pelvic obliquity are to accommodate for the abnormal posture and prevent the abnormality from progressing.
- Fill in the higher side to provide more contact with the seat surface for added stability and even pressure distribution between the lower “at risk” IT and the higher “free floating” IT.
- Build up the higher side to prevent the lower IT from excess pressure with the goal of at least ½ inch space between the lower IT and the seat surface.
To support the scoliosis seen at the trunk:
- Add stability by using a deeper back support that can immerse and capture the abnormal curvatures of the spine. This will also protect the spine from peak pressures that could cause a wound.
- Use mounted laterals to add counter pressure for more midline posture.
- A 3-point system attached to the specialized wheelchair back support cushion may be indicated to correct or prevent further progression of the scoliosis:
- One lateral placed at the thoracic spine at the apex of the curvature
- One lateral placed under the axilla, avoiding direct pressure at the axilla to prevent nerve damage
- One lateral placed lower, close to the pelvis
- Support the head if affected. A head support that gives posterior support in the suboccipital area and has angle adjustability to prevent rotation and lateral flexion of the neck is recommended.
Remember, a pelvic obliquity can sometimes be caused by the seating system we place the resident in. Begin trying to “fix” the problem by ensuring the wheelchair is fit to your resident’s personal dimensions. By following the goals listed above with a resident that sits with an obliquity and a scoliotic spine, you will be well on your way to a successful solution to a difficult seating and positioning case!

Ana Endsjo, MOTR/L, CLT
Clinical Education Manager LTC Division
Ana Endsjo has worked as an occupational therapist since 2001 in a variety of treatment settings. She has mainly worked with the geriatric population, dedicated to the betterment of the treatment of the elderly in LTC centers. Her focus has been on seating and positioning and contracture management of the nursing home resident. With this experience, her hope is to guide other therapists, rehab directors, nurses, and administrators through educational guides, blogs, webinars, and live courses in her role as Clinical Education Manager for the long term care division.