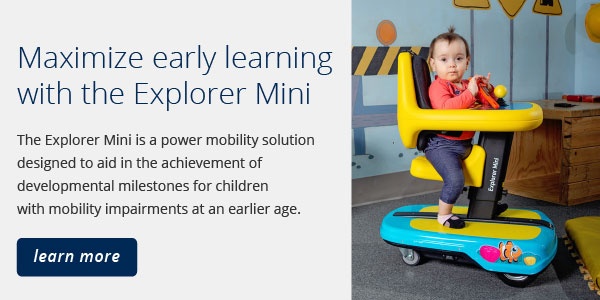
Part 6 in our series about developmental milestones in early childhood focusing on mobility. See part 1, part 2, part 3, part 4, part 5, part 7, part 8, part 9, part 10, part 11, and part 12. Learn more about the Explorer Mini here.
Proximal stability creates distal stability and mobility.
The development of posture begins in utero. As the fetus moves against the uterine wall and encounters resistance and moves through amniotic fluid against gravity, muscle strength and tone develop. The baby finds a sense of self and stability due to proprioceptive input. Proprioceptive input is the pressure to the joints, muscles, and connective tissues that tells us where our body is in space, and this is happening even in the womb.
Fetal movement is spontaneously generated and modifiable based on environmental stimuli. Gibson (1988) uses the term “perception-action” supporting the concept that sensory input elicits motor output in a continual cycle rather than a start stop action. Sensory information, movement variability, and postural control are structural and occur during gestation, after birth and throughout the life span.
Why movement is important
Proprioception is the sense that tells us where the body is in space. Proprioceptive input is a sensation at a joint, muscle or connective tissue that is obtained by weight-bearing, lifting, pushing, or pulling objects. When a child is unable to independently move, this proprioception is impacted which can affect body awareness, self-regulation, posture, and coordination to name a few. This is why the position or posture that we put a young child in is so important. We want to promote postures that will provide proprioceptive input at the joints and allow movement to provide stimuli that will trigger muscle function. It’s important to note that providing static or constant stimuli such as constant pressure to a joint capsule results in adaptation. This means the mechanoreceptors embedded in ligaments and joints adapt to a constant stimulus and stop transmitting information about that joint and muscles will not be activated.
This is one reason movement should not be limited by excessive or undue restraints.
Most early mobility devices include postural supports such as pelvic belts, chest harnesses, head supports. These make sense for a full-time mobility device, to provide appropriate support to facilitate an upright and functional posture. But the Explorer Mini was designed with another objective in mind. This device is not meant to be used full time and was designed to promote developmental milestones through movement—not only movement of the device, but movement of an unrestricted yet safe supported posture.
What does this look like?
You can see below when Davis was first placed in the device he was severely leaning but was not in danger of falling due to the inherent support of the tray and back. The temptation was to “fix” his posture right away and not watch him struggle. Yet we are used to watching typically developing children struggle through their milestones with crawling, sitting, standing, and walking. We watched Davis struggle and he was persistent and moved himself into an upright seated posture where he could eventually have success achieving midline in the device!

The Explorer Mini was designed to promote proprioceptive input to the upper extremities with the tray and joystick, and to the lower extremities with the saddle seat and adjustable seat height.
| Upper Extremity Weight-Bearing |
Weight-bearing through the forearms and hands contributes to weight-bearing at the shoulder joint which translates stability into the upper trunk leading to greater control of the upper trunk and head. This synergistic (combined ) weight-bearing aids in the development of oculomotor stability and vestibular stimuli. |
| Lower Extremity Weight-Bearing | The saddle seat specifically promotes proprioceptive input and hip development by positioning hips in abduction with lower extremity weight-bearing. The seat height can be adjusted to alter joint angles and encourage forward weight shift. Additionally, the shape of the saddle seat coupled with the tray for upper extremity weight-bearing bring the pelvis into an anterior pelvic tilt which encourages trunk extension. |
There are intentionally no postural restraints on the Explorer Mini to allow movement and proprioceptive input to the joints and encourage muscle activation.
The body needs frequent opportunities to move around a stable surface, that being the pelvis and/or lower body support. One consideration in using a device like the Explorer Mini is to alter the positions and height of the tray and seat support to provide a variety of joint angles and maximize proprioceptive input.
The following picture depicts how the table and seat surface of the Explorer Mini facilitates postural support through the multiple weight-bearing surfaces.

Remember, the Explorer Mini is not intended to be a child’s full-time device. It is meant to be a tool that will promotes self-initiated mobility and allow freedom of movement to develop trunk extension and stability, head control, and functional use of the upper extremities. Reach out for a trial today!
1. Hagert, E., Persson, J., Werner, M., & Ljung, B-O. (2009). Evidence of wrist proprioceptive reflexes elicited after stimulation of the scapholunate interosseous ligament. American Society for Surgery of the Hand, 34A. 642-651.
2. Henderson, A., & Pehoski, C., (2006). Hand Functions in the Child: Foundations for Remediation, 2nd edition. Mosby, Elsevier. St. Louis, Missouri.
3. Michelson, JD, & Hutchins, C., (1995), Mechanoreceptors in human ankle ligaments. The Journal of Bone and Joint Surgery. British vol. 77-B
4. Rosenblum, S., & Josman, N. (2003). The relationship between postural control and fine manual dexterity. Physical and Occupational Therapy in Pediatrics, 23,(4). 47-60.
5. Stavness, C., (2006). The effect of positioning for children with Cerebral Palsy on upper-extremity function: A review of the evidence. PT and OT in Pediatrics, 26,39-52
6. Westcott, S., & Burtner, P. (2004). Postural control in children: Implications for pediatric practice. PT and OT in Pediatrics, 24, 5-55.
7. Scheiman, M. (2011). Understanding and managing vision deficits: A guide for occupational therapists. Thorofare, NJ: SLACK Incorporated.
 Dr Teresa Plummer, PhD, OTR/L, ATP, CEAS, CAPS
Dr Teresa Plummer, PhD, OTR/L, ATP, CEAS, CAPS
Associate Professor in the School of Occupational Therapy at Belmont University
Dr Teresa Plummer, PhD, OTR/L, ATP, CEAS, CAPS is an Associate Professor in the School of Occupational Therapy at Belmont University in Nashville, TN. She has over 40 yrs of OT experience and 20 in the area of Assistive Technology. She is a member of the International Society of Wheelchair Providers, and the Clinicians Task Force. She is a reviewer for American Journal of OT and guest reviewer for many other journals. She has presented internationally, nationally and regionally particularly in the area of pediatric power mobility. She has authored journal articles and textbook chapters in the area of OT and pediatric mobility and access.