Part 8 in our series about developmental milestones in early childhood focusing on mobility. See part 1, part 2, part 3, part 4, part 5, part 6, part 7, part 9, part 10, part 11, and part 12.
The Explorer Mini is designed for children with mobility impairments as defined by Hays (1) who has defined the most widely used classification of infant and children’s mastery of functional mobility. These Hays functional groups include:
| Functional Groups | Examples |
| Children who may never ambulate |
|
| Children with inefficient mobility |
|
| Children who lose the ability to walk or to walk efficiently |
|
| Children who need mobility assistance in early childhood |
|
There are hundreds of pediatric medical diagnoses that may warrant the consideration of a power mobility device (PMD). However, there are some limitations of associating the use of a device solely with a specific diagnosis. One consideration is that many children are not diagnosed with a medical diagnosis as no etiology can be pinpointed for the cause of the deficits. In this common situation, a child may demonstrate delays in development but there is no known cause. In these cases, it is not unusual to wait until a child is 24-48 months to deem that this is a delay in development. And we know from our previous blog what happens when a child is unable to perform self-initiated movement. Rather than relying on diagnosis to determine the use of a PMD, it may be prudent to use the Hays (1) categories to determine the need.
A diagnosis such as spinal muscular atrophy impairs a body structure and consequently a function such as sitting and walking. Whereas a diagnosis like developmental delay is not associated with a body structure deficit but rather functional deficits ranging from the inability to reach developmental milestones such as fine motor dexterity to severe deficits in all motor tasks. Some children may have visual problems and some may not. Each case is different.
One may also consider the International Classification of Functioning, Disability and Health (ICF) as a framework for establishing a nomenclature for describing a mobility impairment. The level of impairment can be at the level of health condition, body structure and function, activities, participation, environmental or personal factors. Any one or all of these can lead to a child not having access to mobility and thereby participation (15).
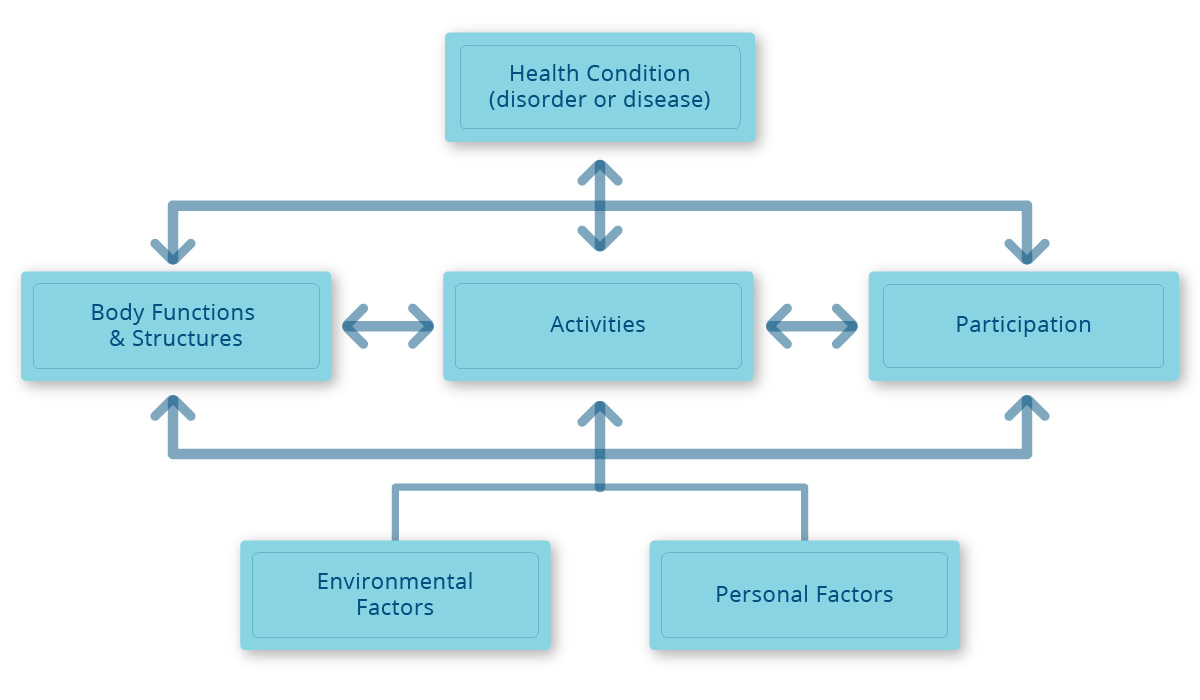
The ICF conceptualizes a person's level of functioning as a dynamic interaction between her or his health conditions, environmental factors, and personal factors. It is a biopsychosocial model of disability, based on an integration of the social and medical models of disability. Disability is multidimensional and interactive. All components of disability are important and any one may interact with another. By way of illustration a graphic depiction may include any of all of the following levels of impairment that may warrant consideration for a power mobility device such as the Explorer Mini (15).
Without an opportunity to participate in life’s activities a child may develop additional impairments and delays. Exploration provides an infant with new perspectives and reveals new information that drive changes in a host of different psychological phenomena (3). For young children with disabilities such as CP, Spina Bifida, and other developmental disabilities, studies have shown that cognitive, social, and language development can be advanced through powered-mobility interventions (10, 13). Whereby a lack of environmental exploration leads to delays in cognition, vision, language and social skills (3). The World Health Organization has recognized that children who experience reduced mobility are at an increased risk of being denied educational opportunities, with the resulting impact on future employment and poverty (4). Therefore, it is imperative that we consider young children with mobility impairments as candidates for the Explorer Mini.
1. Rosen, L., Plummer, T., Sabet, A., Lange, M., & Livingstone, R. (2017). RESNA Position on the Application of Power Mobility Devices for Pediatric Users-Update 201. Rehabilitation Engineering And Assistive Technology Society Of North America
2. Acredolo, L.P., Adams, A., & Goddwyn, SW., (1984) The role of self-produced movement and visual tracking in infant spatial orientation. Journal of Experimental Psychology, 38, 312-327. Doi: 10.1016/0022-0965(84)90128-0
3. Anderson, D. I., Campos, J. J., Witherington, D. C., Dahl, A., Rivera, M., He, M.,… Barbu-Roth, M. (2013). The role of locomotion in psychologicaldevelopment. Frontiers in Psychology, 4(July), 440. https://doi.org/10.3389/fpsyg.2013.00440
4. Armstrong, W., Borg, J., Krizack, M., Lindsley, A., Mines, K., Pearlman, J., . . . Sheldon, S. (2008). Guidelines on the provision of manual wheelchairs in less resourced settings. Geneva, Switzerland: World Health Organization, WHO Press.
5. Butler, P. (1988). High tech tots: Technology for mobility, manipulation, communication, and learning in early childhood.Technology, Infants Young Children, 1, 66-73
6. Butler, P.B. (1998) A preliminary report on the effectiveness of trunk targeting in achieving independent sitting balance in children with cerebral palsy. Clinical Rehabilitation, 12, 281-293.
7. Butler C, Okamoto G and McKay T. Powered mobility for very young disabled children. Dev Med Child Neurology. 1983;25(4):472–474.
8. Butler C, Okamoto G and McKay T. Motorized wheelchair driving by disabled children. Arch Phys Med Rehabilitation 1984;65(2):95–97.
9. Higgins, C. I., Campos, J. J., and Kermoian, R. (1996). Effect of self-produced locomotion on infant postural compensation to optic flow. Dev. Psychol. 32, 836–841. doi: 10.1037/0012-1649.32.5.836
10. Lynch A, Ryu J, Agrawal S, Galloway JC. (2009) Power mobility training for a 7-month-old infant with spina bifida. Pediatric Physical Therapy.;21:362–368.
11. Mancini, M. C., Coster, W. J., Trombly, C. a, & Heeren, T. C. (2000). Predicting elementary school participation in children with disabilities. Archives of Physical Medicine and Rehabilitation, 81(3), 339–347. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10724080
12. Paulsson K Christofferson M - 1986 - Psychosocial aspects of technical aids How does independent mobility affect the psychosocial and intellectual development of children with physical disabilities.pdf.
13. Ragonesi CB, Chen X, Agrawal S, Galloway JC. Power mobility and socialization in preschool: a case study of a child with cerebral palsy. Pediatric Physical Therapy. 2010; 22:322–329.
14. Stanton, D., Wilson, P.N., and Foreman, N. (2002). Effects of early mobility on shortcut performance in a simulated maze. Behavior Brain,136, 61-66. doi:10.1016/SO166-4328 (02)00097-9
15. World Health Organization. (2001) The ICF: An overview. Retrieved from https://www.wcpt.org/sites/wcpt.org/files/files/GH-ICF_overview_FINAL_for_WHO.pdf
16. Weisz JR (1979) Perceived control and learned helplessness among mentally retarded and nonretarded children: a developmental analysis. Developmental Psychology 15(3): 311–9470
 Dr Teresa Plummer, PhD, OTR/L, ATP, CEAS, CAPS
Dr Teresa Plummer, PhD, OTR/L, ATP, CEAS, CAPS
Associate Professor in the School of Occupational Therapy at Belmont University
Dr Teresa Plummer, PhD, OTR/L, ATP, CEAS, CAPS is an Associate Professor in the School of Occupational Therapy at Belmont University in Nashville, TN. She has over 40 yrs of OT experience and 20 in the area of Assistive Technology. She is a member of the International Society of Wheelchair Providers, and the Clinicians Task Force. She is a reviewer for American Journal of OT and guest reviewer for many other journals. She has presented internationally, nationally and regionally particularly in the area of pediatric power mobility. She has authored journal articles and textbook chapters in the area of OT and pediatric mobility and access.

