Part 3 in our Pressure Management Guide series. See Part 1 and Part 2. Check out our comprehensive, digital Pressure Management Guide.
Have you ever been to a ball game and had to sit on those hard bleachers for hours? They are so uncomfortable that stadiums actually sell thin foam cushions to help alleviate pain and discomfort for you to be able to make it through a ball game of two to three hours in length. OR have you had to drive during a long road trip and can barely feel your bottom at the rest stop because it has gone numb? That is why truck drivers often purchase cushions to sit on in their trucks.
What it happening?
The pain that we feel when we sit on a firm, flat surface for long periods of time is due to a buildup of pressure right under our bony prominences. We inherently have bones that stick out and jut down into the support surface that we are sitting on. The most common bones are our “sitting bones,” the ischial tuberosities (ITs). As well, we often slouch and can sit right on our sacrum and/or coccygeal bone.
If we do nothing to protect those bony areas:
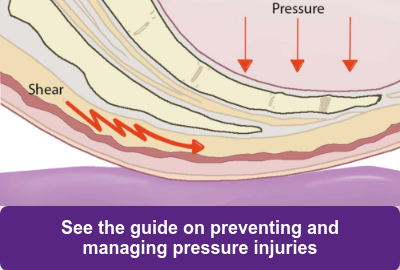
- Pressure builds up, cutting off blood supply, oxygen, and nutrient delivery to that area, leaving the skin and tissue between the seat surface and the bony prominence susceptible to ischemia.
- As we start to feel our bottom go numb, we begin to move and fidget, trying to relieve the discomfort or numbness.
- This movement leads to shear forces that cause frictional forces in conjunction with the downward pressure between the bony prominence and the underlying skin and tissues.
- This not only creates ischemia, but worse yet, tears blood capillaries due to the shear forces.
- This leads to permanent tissue death and a deeper tissue injury.
Similar to how the baseball fan feels after sitting an entire game, our geriatric population who sit not only two to three hours at a time in a wheelchair but six to fourteen hours a day is at higher risk of the same wound development! The elderly population that use a wheelchair as their primary source of locomotion are at an even higher risk than you and I are as able-bodied individuals due to the fact that they cannot get up at will and relieve pressure as necessary. Studies suggest that the elderly population that are wheelchair users are at 36-50% risk of developing a pressure injury.
So, my question is, how can we still have some nursing home residents sitting without a wheelchair seat cushion?
It is our duty as healthcare providers under the Nursing Home Reform Act to, “Ensure that residents do not develop pressure sores and, if a resident has pressure sores, provide the necessary treatment and services to promote healing, prevent infection, and prevent new sores from developing.”
We need to begin to place our residents on skin protection cushions that will:
- increase surface contact area
- distribute pressure away from the high-risk areas under the bony prominences.
Increasing Surface Contact Area:
Pressure can never truly be eliminated, but it can be redistributed to greater surface areas to produce less pressure. So, our goal should be pressure redistribution over the greatest surface area rather than only through small surface areas that would create a high-risk area for a pressure injury to develop.
|
High Pressure
|
Low Pressure
|
| When a force is applied on a smaller surface area, it produces high peak pressures under the bony prominences. | When the same force is applied over a larger surface ares, a lower pressure is produced. |
How do we redistribute pressure in a skin protection wheelchair cushion?
Pressure distribution can be accomplished in one of two ways:
- Immersion
- Offloading
The use of pressure-reducing wheelchair seat cushion designed to maintain tissue integrity through pressure redistribution will reduce the incidence of sitting-induced pressure injuries. Follow along for the next couple weeks to dive more deeply into the principles of pressure redistribution!
Want to learn more about pressure management and the prevention of pressure injuries? See our comprehensive digital Pressure Management Guide.
References:
Turnham, Hollis, Esquire. "Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA)." Health Care Policy and Politics A to Z (n.d.): n. pag. Federal Nursing Home Reform Act from the Omnibus Budget Reconciliation Act of 1987. Web. 9 Aug. 2016. <http://www.ncmust.com/doclib/OBRA87summary.pdf>.

Ana Endsjo, MOTR/L, CLT
Clinical Education Manager LTC Division
Ana Endsjo has worked as an occupational therapist since 2001 in a variety of treatment settings. She has mainly worked with the geriatric population, dedicated to the betterment of the treatment of the elderly in LTC centers. Her focus has been on seating and positioning and contracture management of the nursing home resident. With this experience, her hope is to guide other therapists, rehab directors, nurses, and administrators through educational guides, blogs, webinars, and live courses in her role as Clinical Education Manager for the long term care division.