Summary & References
When we as healthcare providers understand these key principles and address pressure injuries from all support surfaces, then do we have a chance to win the battle against pressure injuries!
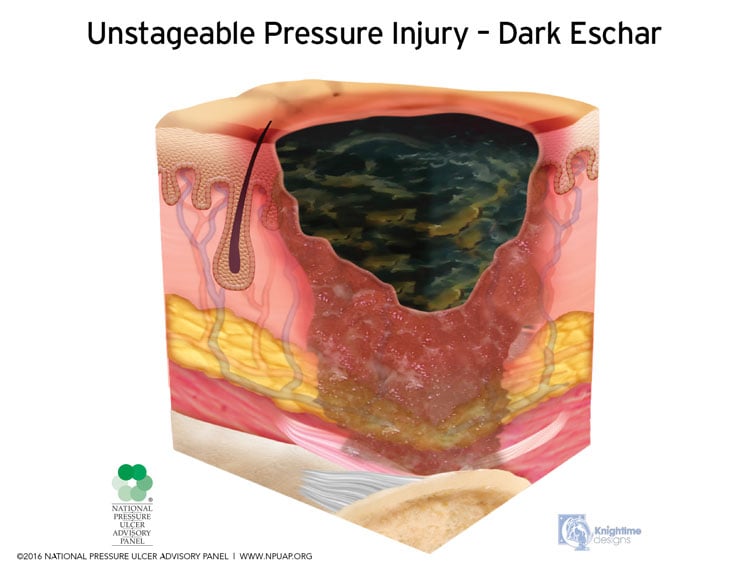
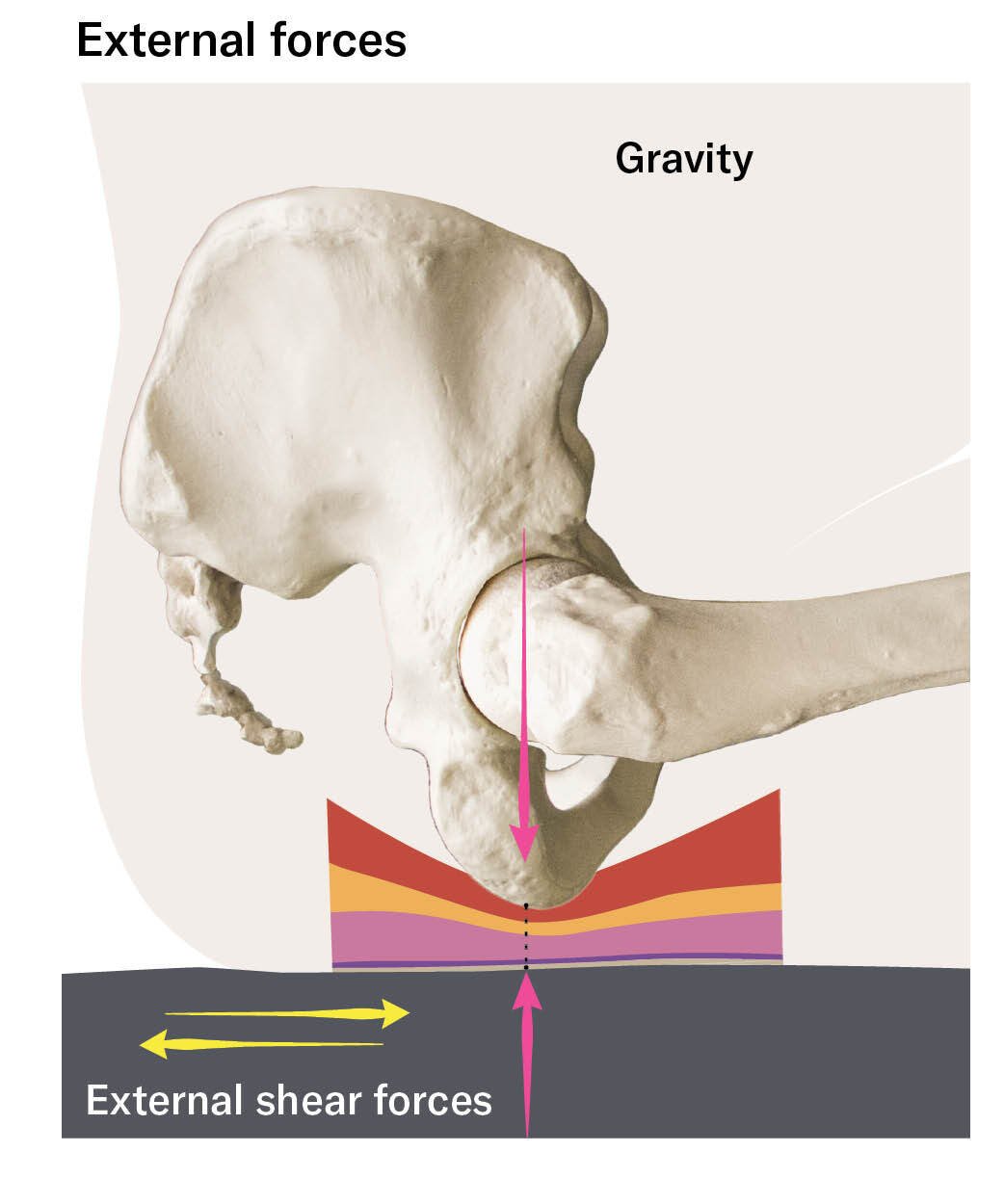
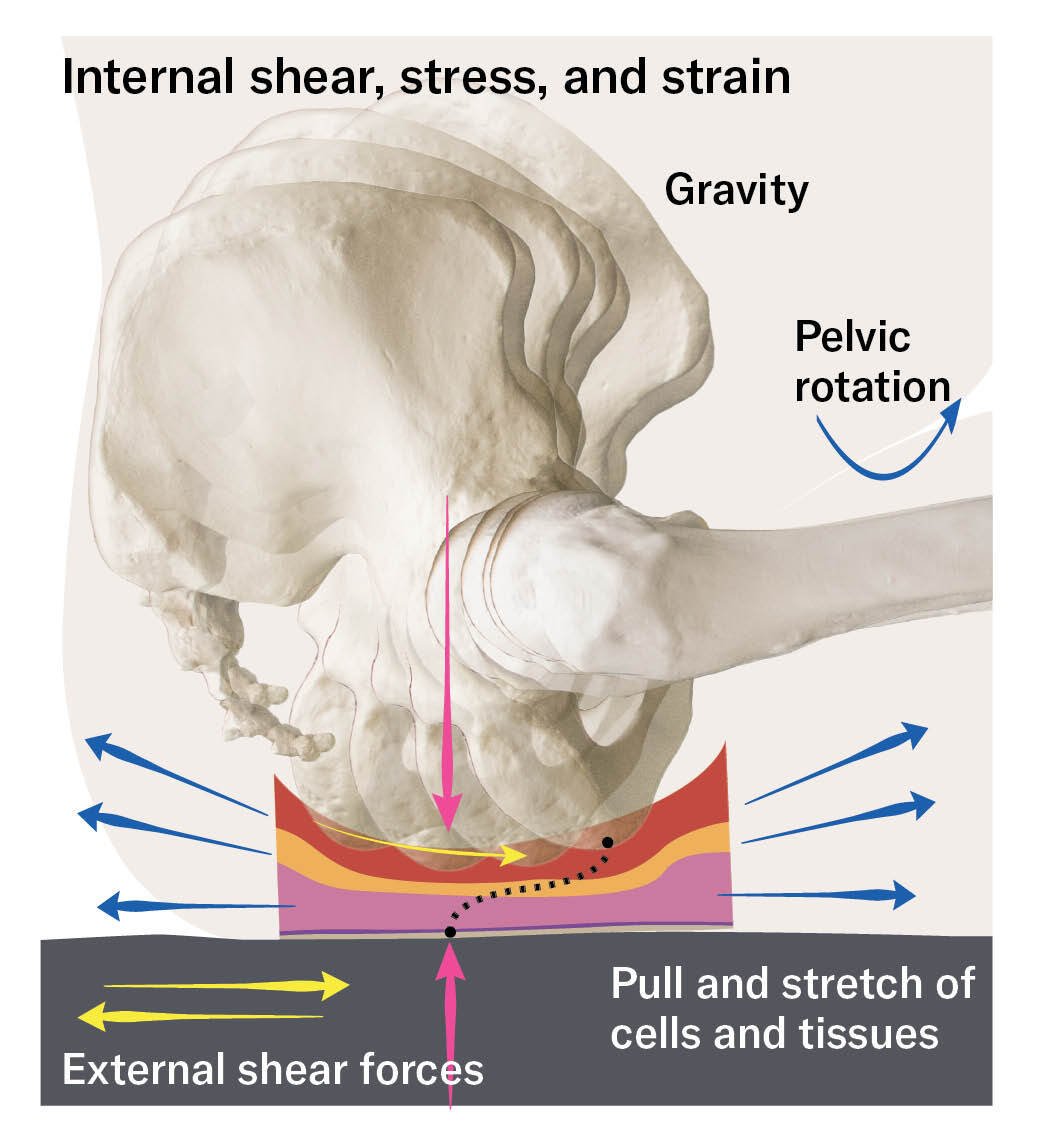
- Appreciate the role of tissue deformation in the formation of pressure injuries.
- Embrace and incorporate the guidance of global experts and authorities on pressure injuries by consulting the Clinical Practice Guideline.
- Understand the intrinsic and extrinsic factors of a pressure injury in relation to the seated posture.
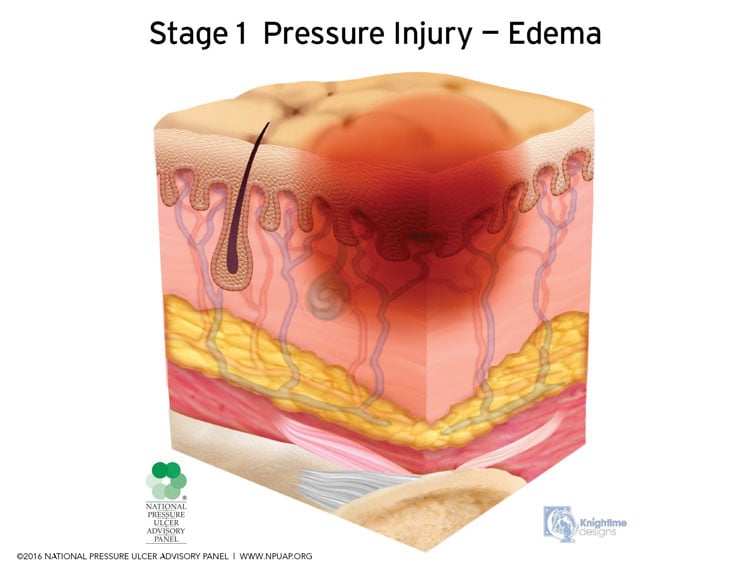
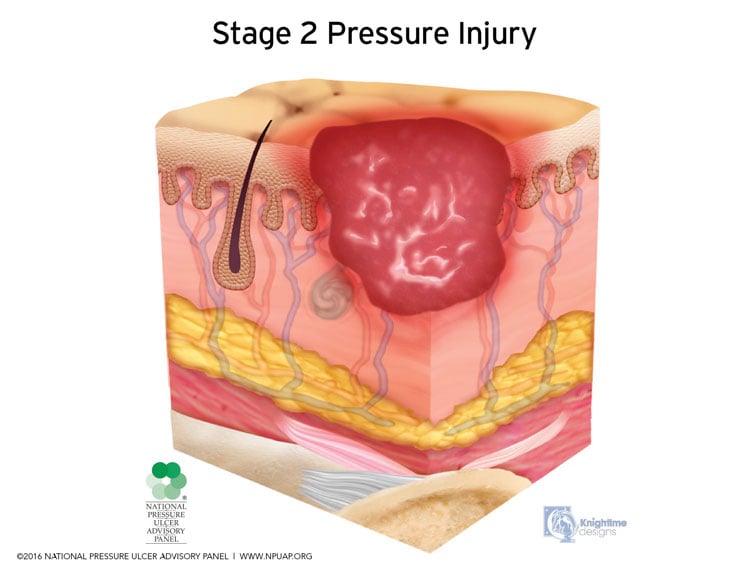
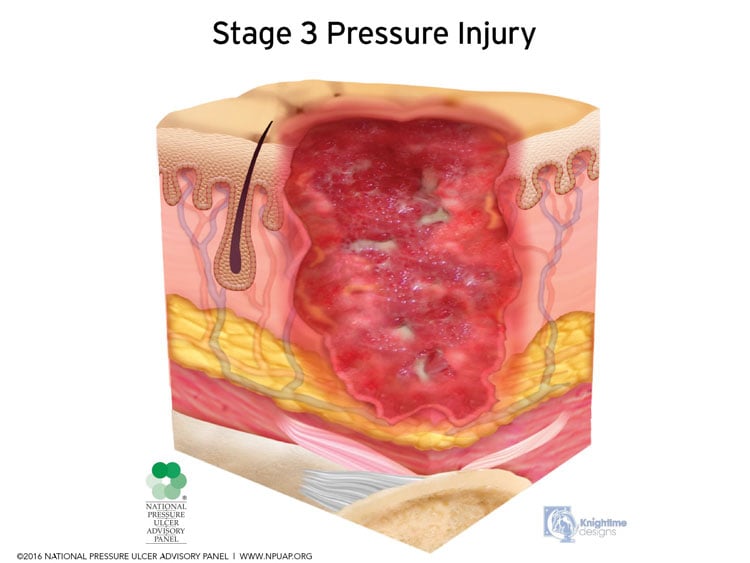
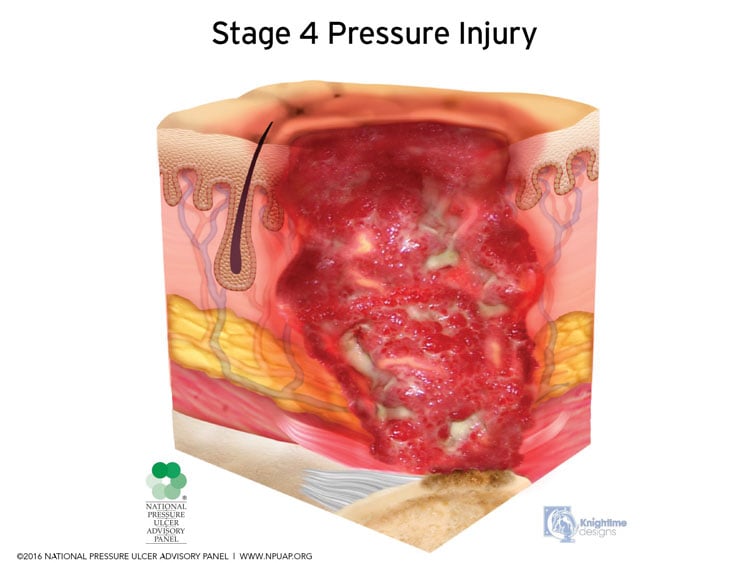
- Educate yourself in the skin changes that make a wheelchair user more susceptible to a pressure injury.
- Understand the critical role addressing the seated posture and all support surfaces play in the holistic approach to the prevention and treatment of a pressure injury.
- Learn the methods of pressure redistribution, the benefits and considerations of each method, and the importance they play in the construction of a cushion and back support to prevent and treat a pressure injury.
- Acknowledge all the components in the simple equation that will result in an optimal seating system.
- Recognize your role, no matter what discipline, in obtaining the appropriate skin protection equipment for the wheelchair system.
Download your free PDF copy of the Pressure Management Guide.
References
European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. "Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline." (2019).
International Organization for Standardization (ISO). ISO 16840, Wheelchair seating – Parts 1-13. International Organization for Standardization. Geneva, Switzerland.
ANSI/RESNA WC-3:2018 American National Standard for Wheelchairs - Volume 3: Wheelchair Seating. Rehabilitation Engineering and Assistive Technology Society of North America. Arlington, VA.
ANSI/RESNA SS-1:2019 American National Standard for Support Surfaces – Volume 1: Requirements and Test Methods for Full Body Support Surfaces. Rehabilitation Engineering and Assistive Technology Society of North America. Arlington, VA.
Gefen, Amit, et al. "Our contemporary understanding of the aetiology of pressure ulcers/pressure injuries." International wound journal 19.3 (2022): 692-704.
Jan, Y. K., Jones, M. A., Rabadi, M. H., Foreman, R. D., & Thiessen, A. (2010). Effect of wheelchair tilt-in-space and recline angles on skin perfusion over the ischial tuberosity in people with spinal cord injury. Archives of physical medicine and rehabilitation, 91(11), 1758-1764.
Jones, D., Radar, J. (2015.) Seating and mobility for older adults living in nursing homes: What has changed clinically in the past 20 years? Topics of Geriatric Rehabilitation, 31, 10-18.
Lange, Michelle L., and Jean Minkel. (2018). Seating and Wheeled Mobility: a Clinical Resource Guide. Thorofare, NJ: Slack Incorporated.
RESNA Position on the Application of Wheelchair Standing Devices: 2013 Current State of the Literature
RESNA Position on the Application of Tilt, Recline, and Elevating Legrests for Wheelchairs: 2015 Current State of the Literature
Sprigle, S., Maurer, C., & Sorenblum, S. E. (2010). Load redistribution in variable position wheelchairs in people with spinal cord injury. The journal of spinal cord medicine, 33(1), 58-64.



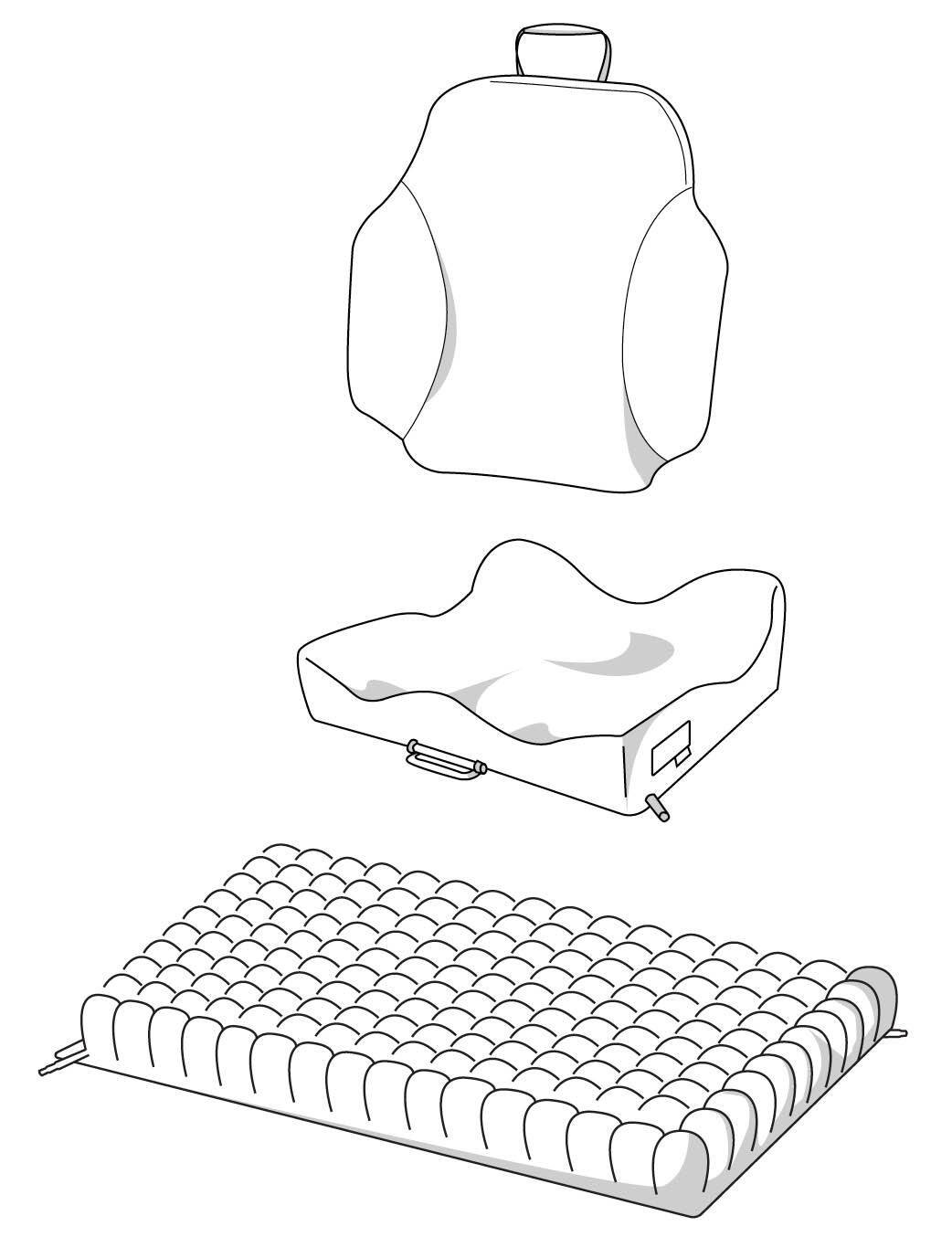











 This relocates higher pressure and increases surface area.
This relocates higher pressure and increases surface area.





