Update your browser to view this website correctly. View list of available browsers
.webp)
This guide is intended to demystify the provision of wheelchair seating and positioning for healthcare professionals. The aim is to assist healthcare professionals in achieving optimal individualized wheelchair seating to meet the goals for each client by:
Understanding the qualifications for both manual and power wheelchairs
Keep in mind this guide uses common therapy terms to keep the concepts as relatable as possible. For the most up-to-date, standardized wheelchair terms and definitions, see the “Glossary of Wheelchair Terms and Definitions” found:
Waugh, K; Crane, B; Taylor, S; Davis, K; Cwertnia, S; Brown, L; Saftler, F; Christie, S. Glossary of Wheelchair Terms and Definitions. Published by the University of Colorado, Assistive Technology Partners, through a grant from the Paralyzed Veterans Association. December, 2013.
This guide is not intended to replace the advice of a medical professional. This guide was created using process and funding guidelines for the United States, including Medicare terminology.
To download the Wheelchair Seating & Positioning Guide as a PDF click here.
Look for these info boxes throughout the guide. They include quick tips or takeaways for that section.
|
ATP: Assistive Technology Professional NP: Assistive Technology Professional PA: Physician Assistant LMN: Letter of Medical Necessity DME: Durable Medical Equipment CRT: Complex Rehab Technology ROM: Range of Motion ADLs: Activities of Daily Living MRADLs: Mobility Related ADLs MWC: Manual Wheelchair |
PWC: Power Wheelchair PPT: Posterior Pelvic Tilt PSIS: Posterior Superior Iliac Spine ASIS: Anterior Superior Iliac Spine IT: Ischial Tuberosity ELR: Elevating Leg Rest STFH: Seat-to-Floor Height LE: Lower Extremity UE: Upper Extremity
|

Chapter 1
In the complicated process of getting seating equipment, it can be hard to even know where to start. Our Wheeled Mobility 101 page goes over the fundamentals of wheeled mobility. Click on the links below to learn more about each topic.
Our manual wheelchair guide and power wheelchair guide go over in detail the topics associated with manual mobility and power mobility. Click on the links below to see each guide.
Chapter 2

When deciding whether or not your patient needs a cushion or back support look at the patient's posture and ask: what is the body doing that it shouldn't be doing? With prolonged sitting, patients begin to shift their bodies into what is known as abnormal postures to seek stability and/or alleviate pain or pressure. It is crucial that you understand what you are looking at and decide whether your goal is to correct or accommodate for the abnormal posture.
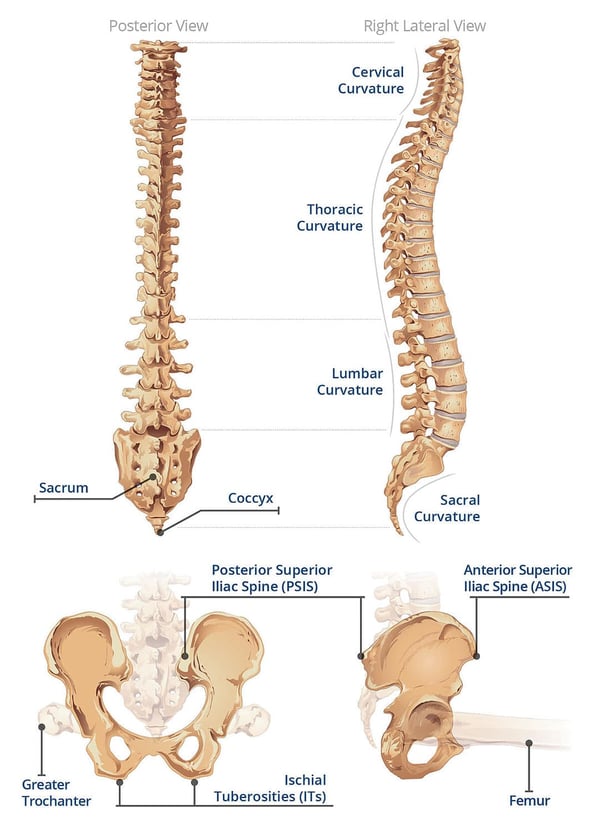
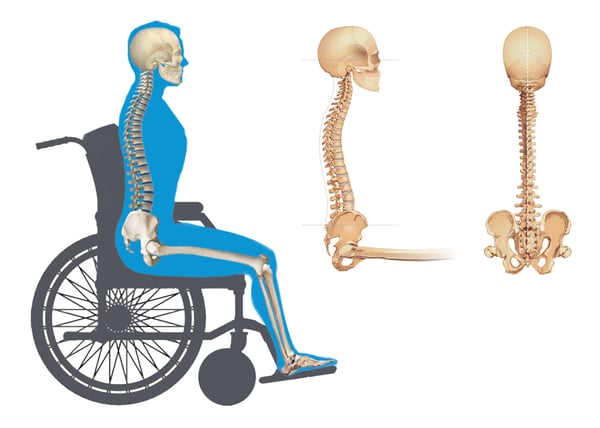
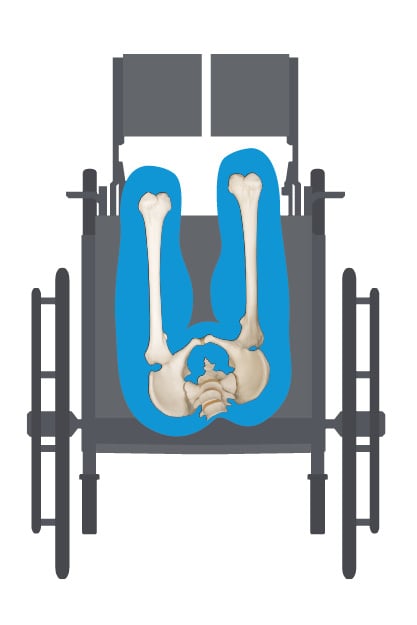
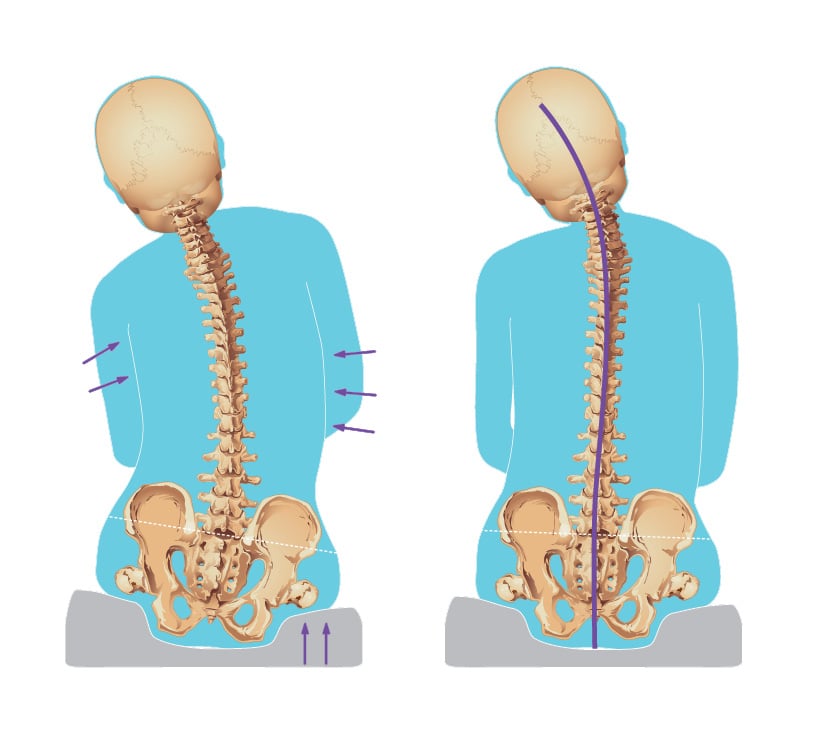
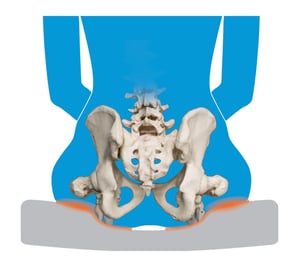
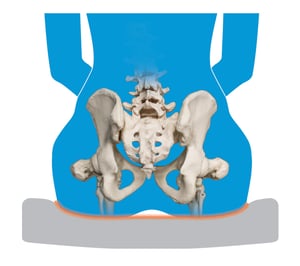
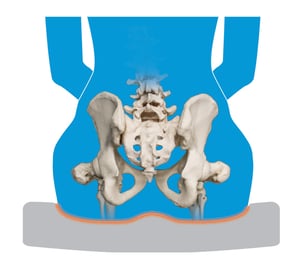
Before we start talking about abnormal postures, let's take a quick look at the spine and pelvis and what a neutral pelvic posture looks like.
Click on any of the abnormal postures to see in more detail what the pelvis, spine, and head are doing in each posture and what goals to strive for in correcting or accommodating the abnormal posture.



Each abnormality is either FIXED/Non-Reducible or FLEXIBLE/Reducible.
Understanding whether the postural abnormality is non-reducible or reducible helps decide if we need to ACCOMMODATE for or to CORRECT the postural abnormality.
When a posture is non-reducible, the skeleton does not move out of that posture. The patient needs equipment that will accommodate the abnormal posture, providing optimal support and pressure redistribution.
GOAL = Preventing further progression
Reducible means that the posture is flexible, or can be changed. However, not all reducible postures can be corrected to neutral.
GOAL = Prevention from becoming a non-reducible posture
The standardized terms in the wheelchair seating world are now Non-reducible for Fixed and Reducible for Flexible.
Why? The term non-reducible better accounts for the potential worsening of a postural abnormality where the previous term "fixed" did not.
The goal when correcting a reducible posture is to achieve their most neutral posture that can be maintained over time with proper support in order to optimize function.
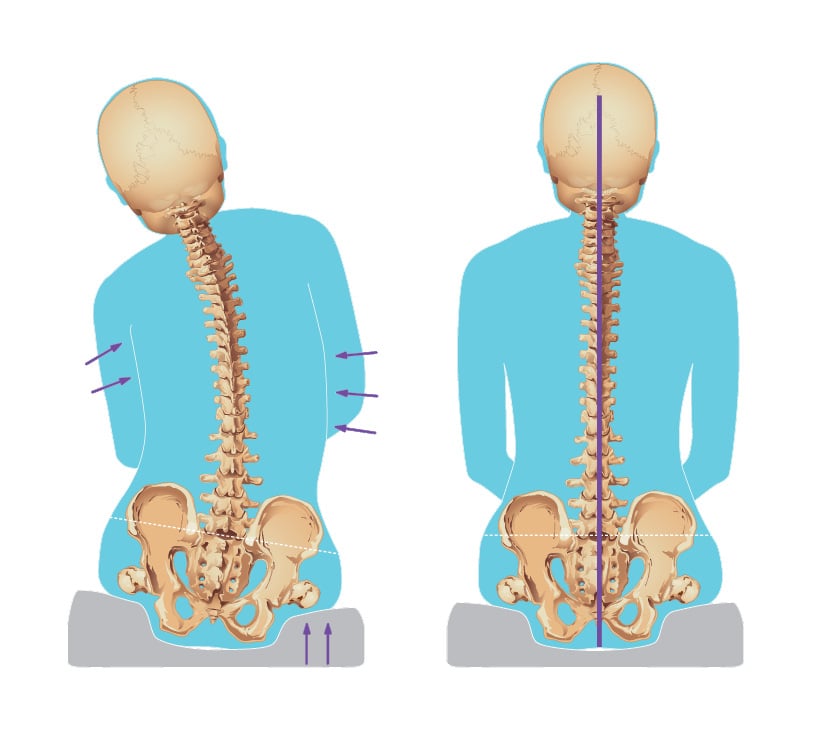
Posture can be moved with support to a neutral/midline position. If they cannot maintain midline over time, the goal is to find the most neutral position for the client and support them to that point.
Even if a client cannot achieve a truly neutral/midline posture, if the posture can be adjusted with support towards midline, it is considered reducible.
With support, if a posture can be moved beyond a neutral/midline position, it is reducible with the goal to position them in midline.
If they cannot maintain the reduced posture over time, your goal may need to shift to accommodating like you would for a non-reducible posture. However, continue to provide interventions that will prevent it from becoming truly non-reducible.
An improper seating system can actually cause or progress abnormal postures.
The wheelchair system can definitely be at fault when the patient is sitting in an abnormal posture. Here is a closer look into seating dimensions and how an ill-fitting wheelchair component can be the culprit behind the body moving into unwanted, harmful postures.
Find out how common seating system issues can affect posture and how to potentially troubleshoot the problems:

Chapter 3
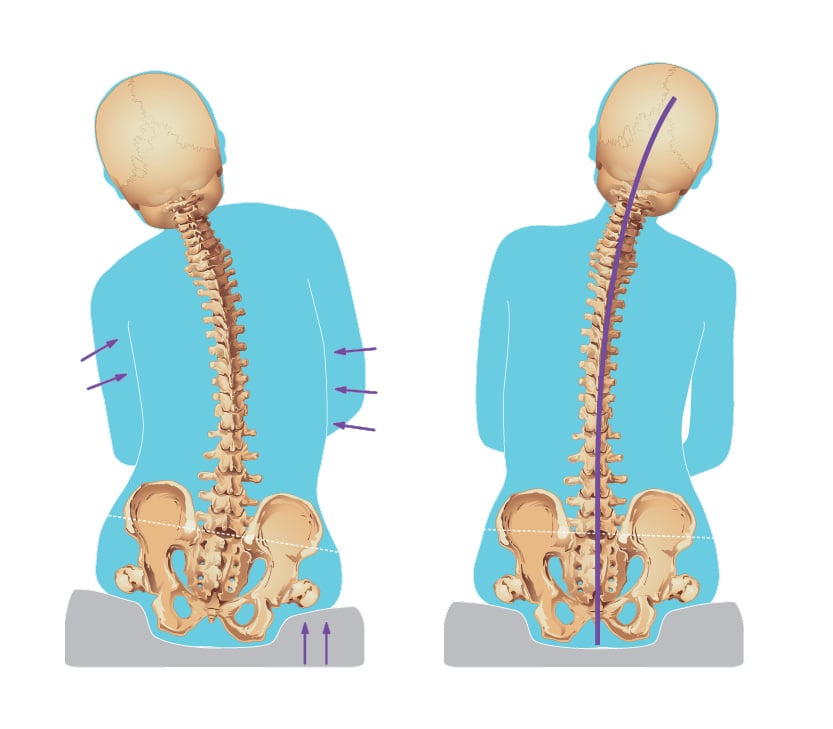
Our beginner's guide to fundamentals of wheeled mobility, Wheeled Mobility 101, goes over the therapy evaluation along with how to measure for properly fitting wheelchair components. We'll go over briefly the measurements. Click on the link below to see the full measurement guide for wheeled mobility.

Chapter 4
Finding the perfect wheelchair cushion for your client can be a daunting task with hundreds of options out there. The first step is knowing what your client qualifies for. This is determined by diagnosis and documented postural presentation. There are resources that can help you find the right code but don't be afraid to ask for help from your trusted ATP/dealer!
Once you know the code, you still have so many options. What then?
There are three areas to understand when choosing a wheelchair seat cushion:
When choosing a cushion, always keep in mind your goals for the pelvis. For example, if the pelvis is in a non-reducible posture, your goal is to accommodate that posture through cushion geometry and medium.
If the posture is reducible, you will look for contours and a medium that can correct the pelvic position.
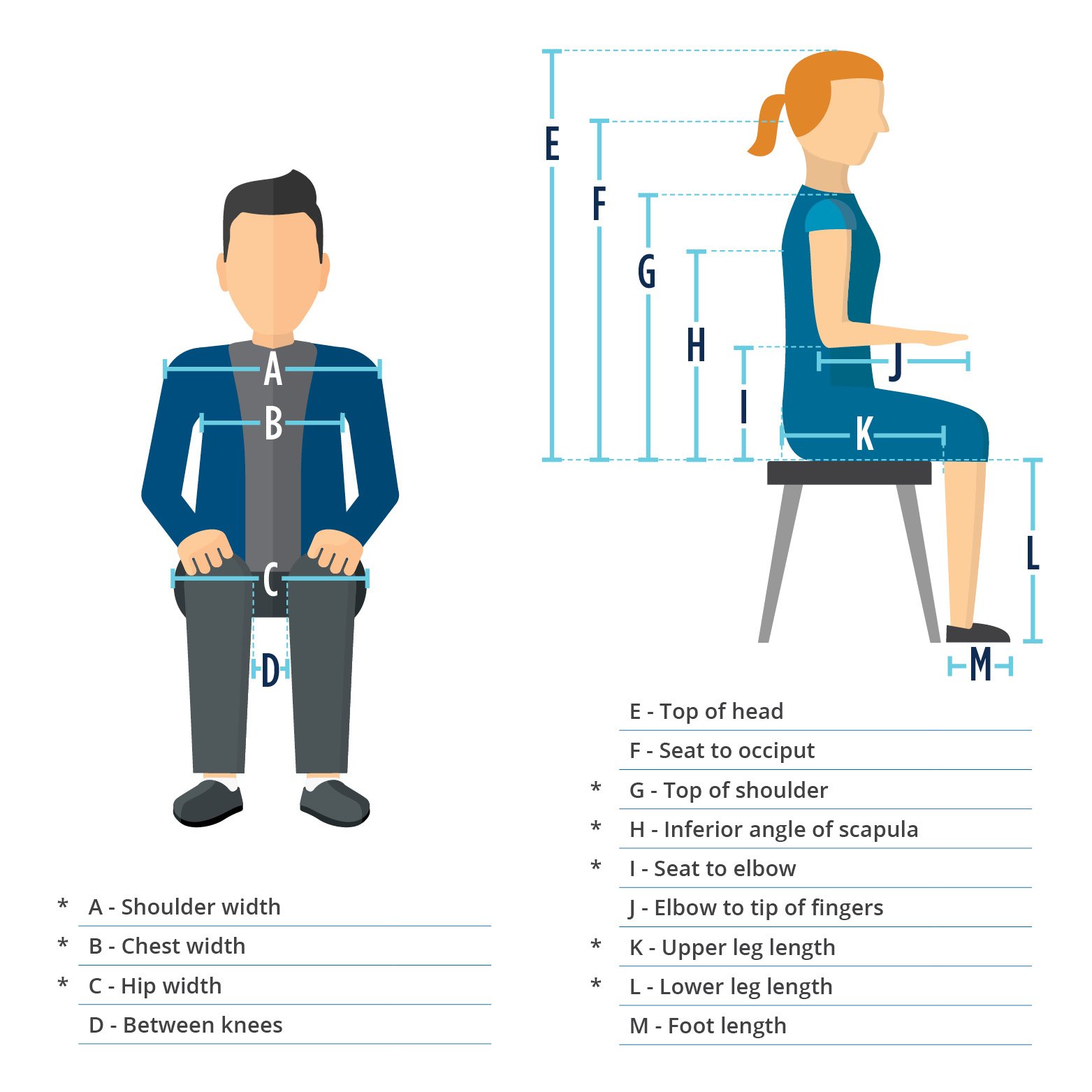
Pressure cannot be eliminated in seating, so instead, we must focus on the redistribution of pressure. Taking the same amount of pressure and spreading it out over a greater surface area will do this (as illustrated below), but even then, there are different methods in doing such.
The principle of taking pressure off of a small surface area and loading it onto a greater surface area that can withstand more pressure and prevent unwanted skin breakdown.
The principle in which a material allows the body to compress or “sink” into it to provide some pressure redistribution with increased surface area contact.
The principle in which a material allows the body to compress or “sink” into it and the material conforms to the body’s shape to provide further pressure redistribution and reduction of peak pressures.
Click on the links below to learn more about each style of cushion geometry along with the benefits and considerations associated with each.

There are different components associated with contoured cushions. Click on each geometric component to learn more.
Understand the available mediums when choosing a cushion. No matter the geometry, the quality of the medium will affect the application of the cushion. Each has benefits and considerations, click on each medium to learn more.
Weight of the cushion
Each medium has different properties, making them lighter or heavier.
Support/stability needs
Each medium has different qualities that make them more or less supportive, which impacts how long a patient can sit in their wheelchair, ease of transfers, and pelvic posture when weakness is present.
Remember to think of the functional and postural goals of your client!
Foam is not foam is not foam! The quality and properties of foam, or any cushion medium, affect the application and effectiveness of a cushion. Be an advocate for your clients and choose QUALITY products!
There are a few key questions to ask yourself when deciding if the manufacturers back support should be replaced with an off-the-shelf back support:
If you answered yes to any of these questions, then, without a doubt, replace the sling back with a separate off-the-shelf back support.
If your patient qualifies for any model wheelchair, they automatically qualify for at least a general use back support. Always consider replacing the sling back with an off-the-shelf option to provide better pelvic and trunk positioning.
The right back support is an essential part of an optimal seating system. Here are some of the important ADVANTAGES of an off-the-shelf back support:
Even when dealing with a more "typical" spinal posture, a solid back support can provide stability to conserve energy for self-propulsion
There are three areas to understand when choosing a wheelchair back support, click on each area to learn more:
As in most things, LESS is MORE and this is certainly true in wheelchair positioning. If you take your time in selecting the right model and size wheelchair and then select an appropriate cushion and back support, accessories may not be needed. Too often accessories are used as “band-aids” for a less than optimal wheelchair seating system. When used the proper way, they can be the finishing touch to achieve the best posture possible for your patient! Below is a list of different types of wheelchair accessories; click on the accessory to learn more.
Chapter 5

There are a few misconceptions that seem to persist in the world of wheelchair seating and positioning. Click on each link below to get an in-depth look at each misconception.
It is important to keep the following goals in mind for your patient both short-term and long-term and then do the best you can!
Click here to download the Wheelchair Seating & Positioning Guide as a PDF
Click here to view the list of references
Remember, there is NO cookbook solution to wheelchair seating and positioning. Use your clinical reasoning skills to figure out what's best within the given parameters.


For more information click here to contact your local representative.
The Wheelchair Seating & Positioning Guide is available for download. Click here to get your PDF copy.
All contents © copyright 2019 Permobil. All rights reserved.
1. Lisa K. Kenyon, Maria Jones, Becky Breaux, Jessica Tsotsoros, Tonya Gardner & Roslyn Livingstone (2019): American and Canadian therapists’ perspectives of age and cognitive skills for paediatric power mobility: a qualitative study, Disability and Rehabilitation: Assistive Technology, DOI: 10.1080/17483107.2019.1606858
2. Whitney, P. G., & Green, J. A. (2011). Changes in infants’ affect related to the onset of independent locomotion. Infant Behavior and Development, 34 (3), 459–466. https://doi.org/10.1016/j.infbeh.2011.05.001
3. Stavness, C., (2006). The effect of positioning for children with Cerebral Palsy on upper-extremity function: A review of the evidence. PT and OT in Pediatrics, 26,39-52)
4. Kenyon, L. K., Schmitt, J., Otieno, S., & Cohen, L. (2019). Providing paediatric power wheelchairs in the USA then and now: a survey of providers. Disability and Rehabilitation: Assistive Technology, 1-10. https://www.tandfonline.com/doi/abs/10.1080/17483107.2019.1617358?journalCode=iidt20