Having limited mobility places a person at high risk for a pressure injury or often what people refer to as a wound. According to the 2021 Fact Sheet: Above Pressure Injuries in US Healthcare, there are 2.5 million cases of pressure injuries per year, and it is the second most common diagnosis in health system billing records in the US.1
Prevention of a pressure injury is key. But what happens when you get one? It can be frustrating, scary, and even alter your life. If you’re used to being up and active and now have to limit your sitting time, that can prevent you from doing your individual activities. We’ve complied our top 10 tips for pressure injury and wound care to help you better understand the many factors that go into healing.
This is not meant as medical advice; we recommend reaching out to your healthcare professional to assess and recommend the best plan for your individual wound care needs.
- Pressure relief: The most crucial step in healing a pressure injury is to relieve the pressure on the affected area. This means avoiding putting pressure on the wound to prevent further damage. Frequent repositioning or using specialized support surfaces can help distribute pressure and reduce the risk of new skin breakdown from forming.
- Wound Cleaning: Keep the wound clean to prevent infection. Seek advice from a healthcare professional and avoid using harsh chemicals or solutions that may irritate the wound.
- Moist Wound Healing: Moist wound healing has been shown to aid in tissue repair. Use appropriate wound dressings that promote a moist environment, which can help accelerate the healing process. Your healthcare professional can recommend the proper care and wound supplies to use!
- Debridement: If the pressure injury has necrotic (dead) tissue, debridement or removal of the necrotic tissue may be necessary. This involves removing the dead tissue to allow healthy tissue to grow.
- Topical Treatments: Depending on the wound's severity and characteristics, healthcare professionals may prescribe specific topical treatments or ointments to promote healing and prevent infection.
- Nutrition: Proper nutrition is essential for wound healing! Make sure you are getting adequate amounts of protein, vitamins, and other nutrients necessary for tissue repair.
- Pain Management: Pain management is important for the comfort of the individual with the pressure injury. Address pain as needed under the guidance of a healthcare professional.
- Manage Underlying Health Conditions: Address and manage any underlying health conditions that may hinder the healing process, such as diabetes or circulatory issues. These can affect and often slow the healing process.
- Regular Assessment: Regularly monitor the wound's progress and healing status. If there are any signs of infection or deterioration, seek medical attention promptly.
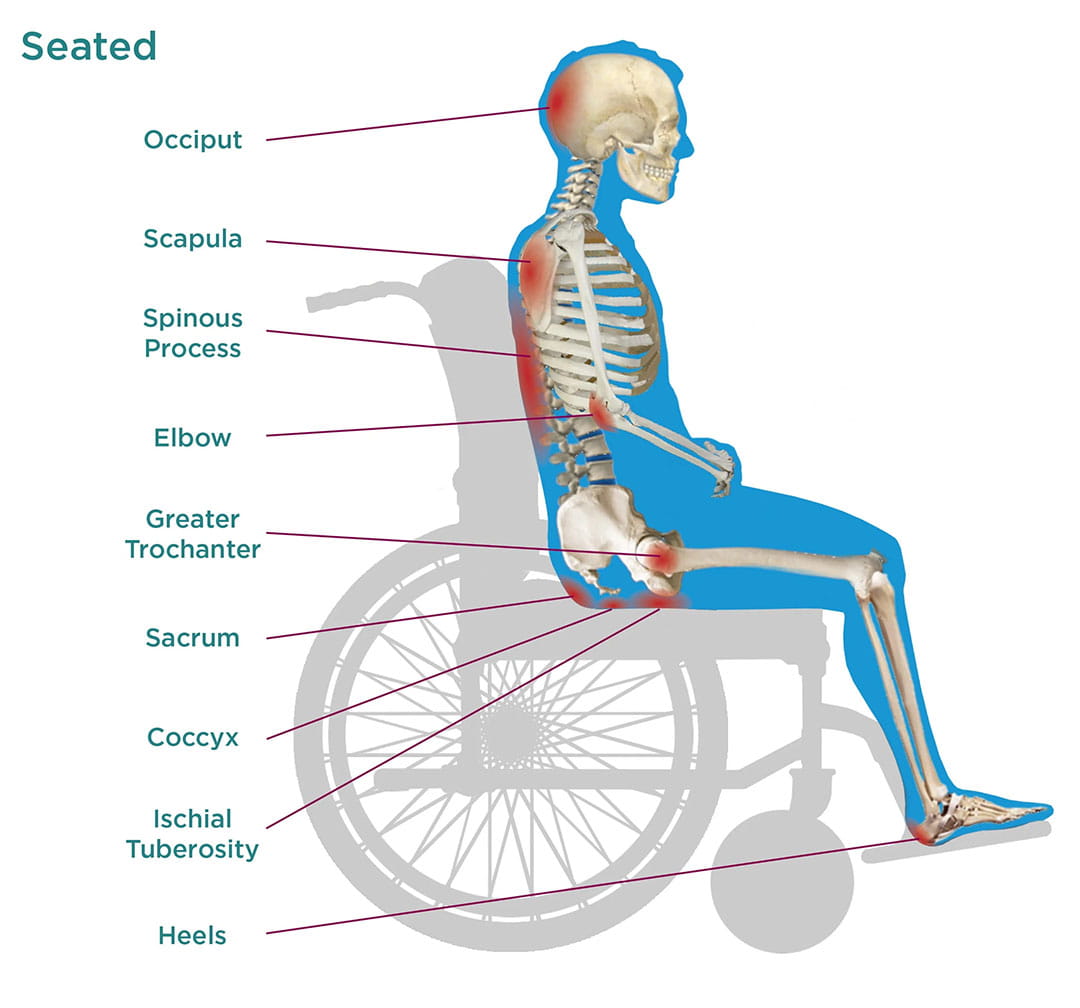
- Consult a Healthcare Professional: For severe or persistent pressure injuries, it's essential to consult a healthcare professional, such as a wound care specialist or a healthcare provider with expertise in treating pressure injuries. If you utilize a wheelchair, you should also reach out to your physical or occupational therapist and DME supplier to assess your current equipment to make sure it’s continuing to meet your seating and positioning needs. Having your equipment pressure mapped can provide insight as well!
It's important to note that the management of pressure injuries may vary depending on individual factors, so always follow the guidance and recommendations of healthcare professionals for the best outcome. Prevention is so crucial, especially for individuals at risk of developing pressure injuries, as they can be challenging to treat once they occur. Regularly assessing those that are at risk and implementing preventative measures can help reduce the incidence of pressure injuries!
Want to learn even about pressure management? Click here to download Permobil’s free Pressure Management Guide.
References:

 Nicole LaBerge, PT, ATP
Nicole LaBerge, PT, ATPPortfolio Marketing Manager - Seating & Positioning
Nicole B. LaBerge, PT, ATP is a Physical Therapist with 17 years of experience in a variety of clinical settings. She currently works for Permobil as a Portfolio Marketing Manager of Seating and Positioning products. Her past clinical practice has included seating and mobility for adult and pediatric populations, with a focus in neurological rehabilitation, power standing and wound care. Nicole has presented at the State and International Levels, has multiple publications in peer reviewed journals and enjoys sharing her passion for patient advocacy, efficiency, and clinical outcomes. She currently serves as an Executive Board Member for the Clinician Task Force.