In this series we're taking a closer look at justification and clinical tips for a few seating and positioning accessories. See last week's post on head supports here.
Why are lateral upper leg supports used?
As therapists we often use the principle of “less is more,” especially when it comes to seating. We will do our initial evaluation and determine the appropriate wheelchair model, seat cushion and back support. Ideally, this will be enough to provide stability, function, and comfort for our client, but sometimes we need more. There are times when the use of a lateral upper leg support can be used to promote that stable base of support, which allows optimal function and comfort. Below are examples of when to consider using lateral upper leg supports. Although the list is not exhaustive, it provides clinical scenarios to consider when they may be appropriate.
Clinical Examples:
- Abnormal tone of lower extremities: In cases of high tone, or low tone, the lower extremities may need a boundary to maintain an optimal position for stability and function.
- Reducible postures: When the lower extremities are not in optimal alignment and there is flexibility in the posture, lateral upper leg supports can be used to minimize the progression of an abnormal posture.
- Progressive diagnoses: Particularly with progressive neurological diseases, a client may sit well for the first couple of hours in their wheelchair. As the day progresses, muscles fatigue and can result in abduction of the lower extremities, which can decrease stability and function. Lateral upper leg supports can be used to promote lower extremity stability.
- Decreased pelvic stability: Consider a unilateral hip disarticulation, and the resulting instability at the pelvis. A lateral upper thigh support can be used to provide a boundary for that upper leg and promote improved pelvic stability.
How to choose a lateral upper leg support
Once you’ve determined that your client will benefit from lateral upper leg supports, there are two things to consider: the pad, and the hardware.
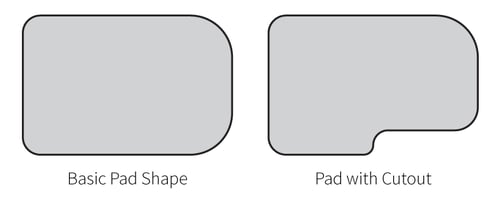
- The pad: When choosing the pad, consider the clinical presentation and what your goals are. Note that there are pads of various lengths that can accommodate various distributions of pressure. For example, if you only need contact at the proximal hip area, then a shorter pad may be sufficient. If you have a client with high tone, you may want to provide a longer pad to distribute pressure over a larger surface area. Also note that there are pad options that have a cut-out to accommodate for the cushion.
- The hardware: Assessing hardware options is critical as this is what gives you adjustability and pad placement. For example, if you have a client that has a windswept posture, you need hardware that allows for angled pad placement to the left or to the right. Another feature to look for is a joint that allows you to angle the pad upwards or downwards. This allows you to make more intimate contact with the upper leg, at the angle needed for optimal support.
Criteria and Justification
Let’s go over how to successfully justify lateral upper leg (pelvic/thigh) supports under Medicare criteria. We’re first going to take a look at what the Medicare criteria is, and then we’ll go over a few sample justifications for lateral upper leg (pelvic/thigh) supports.
The HCPCS code for head support is E0953 and the criteria is as follows:
Medicare Criteria:
Has significant postural asymmetries AND one of the qualifying diagnoses for positioning back support.
For qualifying diagnoses, use the diagnosis search found at https://www.comfortcompany.com/icd_decision_tree. The examples below describe types of postural asymmetries that would meet the Medicare Criteria:
- Compensate for decreased stability and balance due to decreased strength (poor endurance, abnormal tone, poor motor control, other) and allow increased ability to participate in ADLs and IADLs (eating, operating / propelling his wheelchair, performing personal care, using his computer/AAC device/EADL, writing, reading, others)
- Help correct (accommodate) his/her spinal kyphosis (other spinal deformity) and promote an upright posture
- Prevent recurrence (progression) of his/her spinal kyphosis (other spinal deformity)
- Provide increased pressure distribution across the posterior trunk to decrease the risk of pressure injuries on his vertebrae
By describing your individual client’s physical presentation as in the examples above, you are painting a word picture for the reviewer. In addition to describing the postural asymmetries, include a description of why your client needs the lateral upper leg support. The justifications provided below are examples only and are not all-inclusive. Use these as a guide and tailor them to describe the clinical indications of your individual client.
Sample justification for BodiLink Lateral Upper Leg (pelvic/thigh) Supports
Necessary to provide the client with specific support to the lateral aspects of the knee and/or upper leg to:
- Correct (prevent further progression of) his/her tendency to fall into hip abduction and external rotation due to LE weakness (abnormal tone, poor motor control poor endurance, fatigue, pain, other)
- Provide midline LE alignment and increased pressure distribution to the femurs to reduce his/her risk of pressure injuries due to (list specific risks for this person)
Another common accessory used to achieve optimal stability and function in a wheelchair seating system is lateral trunk supports. Check out next week’s blog as I will discuss clinical indications and justification for lateral trunk supports!

Stacey Mullis, OTR/ATP
Director of Clinical Marketing
Stacey is Director of Clinical Marketing. She graduated from Western University in London, Ontario, Canada with a BA Linguistics and BSc Occupational Therapy and has practiced as an OTR for over 20 years. With experience in pediatrics, inpatient/outpatient rehabilitation, long term care, and home health, Stacey has faced the challenges first hand of providing appropriate seating in various clinical settings. This led her to pursue an apprenticeship at Care Partners Seating Clinic in Asheville, NC to advance her skills, and she obtained her ATP certification in 2012. Mullis is a member of the NCOTA, CTF, NRRTs, RESNA, and AOTA.

