Part 3 in our series focusing on wheelchair solutions for Veterans. See Part 1 and Part 2.
The Reality of Chronic Pain for Wheelchair Users
Chronic pain is an unfortunate fact of daily life for many wheelchair users. Sometimes the pain is related to an injury, and other times it is related to being in a wheelchair for extended periods of time. Thankfully, there are some very effective pain management options available to wheelchair users.
1. Equipment
One of the most important things to look at is the existing wheelchair equipment and configuration. We spoke in the first blog about the importance of choosing the lightest wheelchair possible. These are called ultra-lightweight wheelchairs. And if you use manual mobility, then this is true: the weight of the wheelchair frame is critical. But you may be a power wheelchair user and weight doesn’t matter. What other factors contribute to pain?

Clockwise from left: Acta-Relief, Swing-Away Amp, and ROHO® ENHANCER® Cushion
Seat Cushions
If you’ve been a wheelchair user for a long time, you may have tried several seat cushions already. And if you have found one that provides good stability and skin protection for your day-to-day routines, then don’t change it! Unfortunately, many wheelchair users still struggle with pain and may even continue to have skin issues on their current cushion. I encourage you to meet with your seating specialist first so that he can evaluate all the possible reasons and present your options–there are many! In the meantime, here are a few things for you to know about seat cushions.
- There are two main principles of skin protection: Offloading and Immersion/Envelopment. All skin protection cushions will use one of these principles in its construction. Your total presentation will determine which method will work best for you. Discuss this with your seating specialist and trial the different types.
- Stability matters: What I mean by this is that when you try a cushion in a clinic for 30 minutes, it may feel great for that 30minutes, but what about throughout the day? Do you get tired by lunchtime with back pain and need to lie down? It may be that your trunk is working hard all morning since the base you are sitting on is not stable enough. Talk to your therapist about your activity level and what you notice as the day goes on.
- Materials Matter: There are all kinds of seat cushion material technologies. When considering each, always look at the weight (fluid and gel are usually heaviest) and look at the stability of the medium. The weight of a cushion can impact the efficiency of wheelchair propulsion for an active wheelchair user, which can result in shoulder pain. Stability is especially important for someone with upper body weakness like the example mentioned above. So don’t assume that a “softer” cushion will equal decreases pain. A seating specialist can help you find a medium that will work best for you!
Back Rests
And just like you would never get dressed for the day and choose a shirt with no pants, you should never select a seat cushion without considering the back rest. This component is key in providing stability and support in the seated posture. Think about it: when you are in the seated posture your back carries 40-90 % more stress than in standing and must work to keep your trunk upright. If those muscles have been compromised by illness or injury, this becomes even more difficult and can result in abnormal postures and even pain.
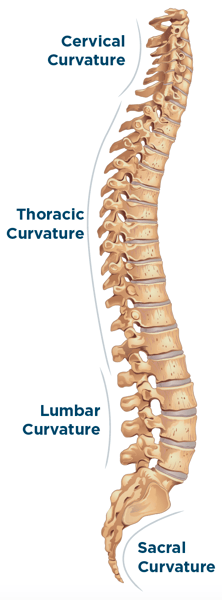
The spine has natural curves in the lower lumbar region, the mid thoracic region, and the cervical region. If not supported, the curves will either flatten or increase. A good back rest will be able to support and maintain those natural curves of the spine. In some cases, a low back rest is enough to provide support in the lumbar region, which has a domino effect of maintaining the other natural curves of the spine. In other cases, the entire trunk needs to be supported and those natural curves need to be “created” by using adjustable components in the back rest. The goal is to determine how much support is truly needed to maintain natural curves and then matching that need with the proper back rest.
Another feature of the back rest is the seat-to-back angle setting. Most wheelchairs have back canes set at a 90 degree angle from the seat surface but not everyone can sit at a 90 degree angle for long periods of time.By opening the seat-to-back angle using back rest hardware, you can increase overall pressure redistribution, which can take pressure off the back and seat surface.
If you’re experiencing pain, have your seating specialist look at your combination of wheelchair, seat cushion, and back support, and ask him to look at your seat-to-back angle. The wrong combination could be causing unnecessary back pain.
2. Pressure Relief
Your ability to re-position and pressure relieve can have a big impact on your level of chronic pain. For example, something as simple as leaning forward all the way can relieve pressure that causes pain at the seat surface. These pressure-relieving techniques are critical when sitting for prolonged periods. Talk to your seating specialist about determining the best pressure-relieving technique for you and developing a daily routine of pressure relief. This can help prevent painful pressure injuries and force you to move throughout the day.
3. Posture Breaks and Stretching
We all can develop bad postural habits over time, and this can be especially true with wheelchair users. You may have developed some bad habits over time in relation to your seated posture and this can sometimes become a source of pain. Intentionally changing your posture can be accomplished by using the right wheelchair, cushion, and back support which we’ve already discussed above. In addition to choosing the most appropriate equipment, a good stretching program may help. If you’ve been sitting in a poor posture for a period of time, your muscles mayhave adjusted to that posture. To change that posture you may need to retrain your muscles! There are stretches that can be done while you’re in your wheelchair during the day as well as in the bed at the beginning or end of your day. Talk to your therapist about whether a daily stretching program and schedule may help to retrain your body to achieve your optimal pain-free posture.
Another simple thing to do, especially if you work at a desk and computer, is to take posture breaks. Just take a minute or two every thirty minutes or so and check your posture. Just like pressure relieving,do a couple of your stretches prescribed by your therapist, or just re-position yourself to a better position. These new habits can help keep you pain-free.
One More Thing: Common to Veterans
When dealing with chronic pain, there may be factors other than those listed above that contribute to the problem. A factor far too common among veterans is leg amputation. If you have had one or both legs amputated, your body automatically experiences a shift of balance and will search for a posture to re-establish that balance. In this case it is critical to select equipment that will provide the most stability in your optimal posture and the most pressure re-distribution. Since a leg or both legs may not be making good surface contact it is important to have a cushion that will maximize contact with the residual limb/s. It’s equally important to have the back support angle set to share some of the pressure distribution and provide the stability your body is searching for.
The good news is that Permobil has equipment options for both manual and power mobility that may help minimize your chronic pain! Check out the selections and technology designed to help you live your best life.

Stacey Mullis, OTR/ATP
Director of Clinical Marketing
Stacey is Director of Clinical Marketing. She graduated from Western University in London, Ontario, Canada with a BA Linguistics and BSc Occupational Therapy and has practiced as an OTR for over 20 years. With experience in pediatrics, inpatient/outpatient rehabilitation, long term care, and home health, Stacey has faced the challenges first hand of providing appropriate seating in various clinical settings. This led her to pursue an apprenticeship at Care Partners Seating Clinic in Asheville, NC to advance her skills, and she obtained her ATP certification in 2012. Mullis is a member of the NCOTA, CTF, NRRTs, RESNA, and AOTA.

