Part 2 in our series about Power Assist Devices. See Part 1 here. Click here to learn more about SmartDrive, Permobil's power assist device.
This week we are continuing our blog series on power assist devices. Last week we looked at contributing factors to upper extremity impairment in manual wheelchair users, and this week we will be focusing on how to determine if a power assist device would be beneficial to you or your clients.
Wheelchair Power Assist Devices and Mobility Related Activities of Daily Living
Power assist devices can be a great solution for mobility related activities of daily living (MRADLs). For example, use of a power assist device may be helpful when carrying objects, grocery shopping, pushing a baby stroller, going up ramps or hills, mopping, sweeping, or when negotiating thresholds or carpet. In addition to MRADLs, a power assist device should also be considered for other life participation goals (e.g., work, school) and recreational activities.
ICF Model
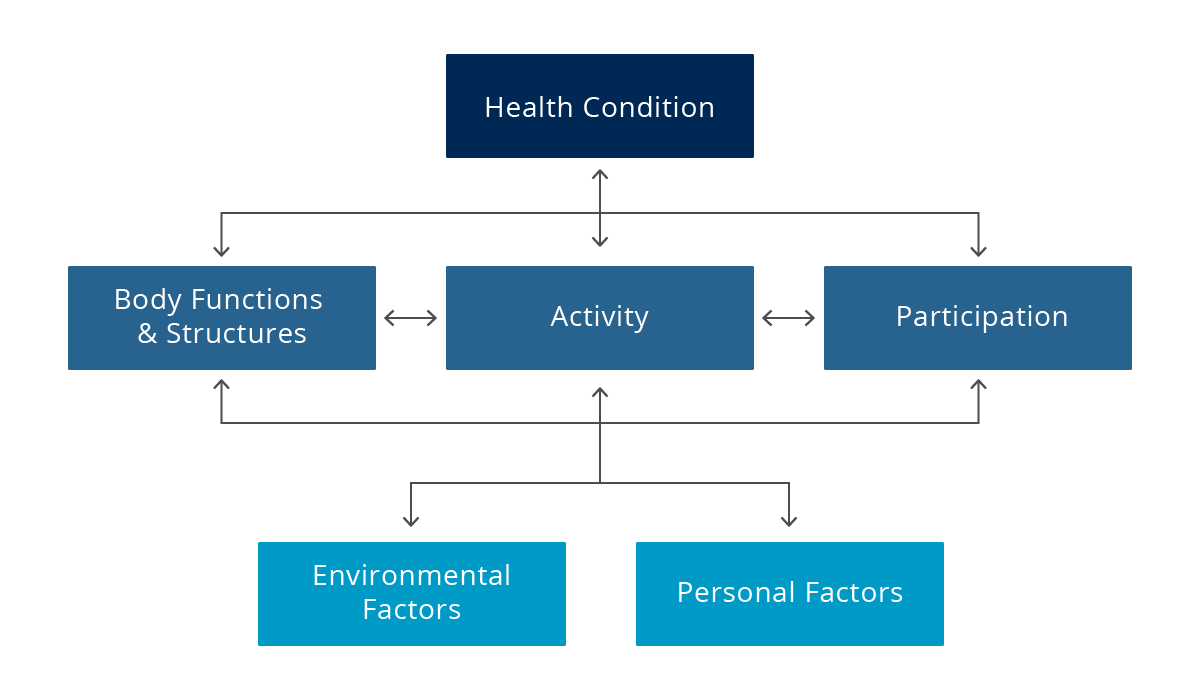
When considering the evaluation process for complex rehab technologies (CRT) including power assist devices, the International Classification of Functioning, Disability, and Health (ICF Model) provides a nice framework from which to work. This framework is what the World Health Organization (WHO) uses to measure health and disability, both at an individual level and population level. The ICF was adopted in 2001, and has been used as a guiding framework since that time (World Health Organization, 2001). When an individual has a health condition resulting in the need for a piece of CRT a clinician, typically an occupational or physical therapist, is involved in evaluating impairments in body functions and structures that are impacting the individual’s performance of daily activities and life participation. Clinicians then work in conjunction with the entire team – client, family members, supplier – to identify what type of CRT will maximize the client’s independence and functional needs throughout the day.
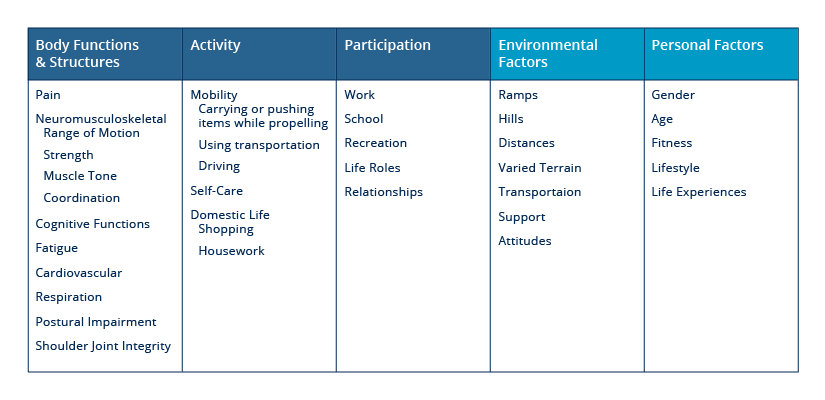
When using the ICF framework to evaluate whether a power assist device is appropriate for someone, here are several factors related to body functions and structures to consider:
- Upper extremity pain
- Limited range of motion
- Limited strength or endurance
- Compromised muscle tone, whether increased or decreased tone
- Difficulties with coordination
- Does the individual have safe reaction times?
- Is fatigue a factor throughout the day or week?
- Are there any cardio pulmonary insufficiencies that are negatively impacted by physical activity?
- Does the client present with postural impairment that may be worsened by their propulsion technique?
We can also look at the benefits of a power assist device when thinking about daily activities. In regards to self-care, can the individual get to the bathroom in time to prevent an incontinent episode? Is the ability to carry things while propelling a manual wheelchair a need? Likely the answer is yes! We also need to consider the individual’s life participation. What are their roles in life and how have those roles been impacted by a mobility impairment? How far does the individual have to propel day to day in order to do what they need and want to do? What types of environments are encountered? And can all of these activities and roles be carried out to the extent that the individual wants? During these activities and roles, is mobility as independent, efficient, and safe as possible? As you can see, it isn’t just upper extremity impairment that creates the potential need for power assist. We have to think about that big picture, both from a physiological standpoint as well as from a daily participation and functioning standpoint.
Who is Appropriate?
If you are a manual wheelchair user, or work with manual wheelchair users, and you or your client has the ability to safely operate a power assist device, consider trying it. When considering safe operation, understand that safe use requires training and a safe environment in which to learn. Also know there are options for programming and activation to help meet different individual user’s needs.
If you are wondering if power assist may be right for you or one of your clients, , consider the following questions :
- Are you a long-term manual wheelchair user?
- Do you have a history of upper limb pain or dysfunction?
- Have you experienced fatigue with manual wheelchair mobility?
- Do you experience changes in oxygen saturation with increased physical activity?
- Do you require more than a manual wheelchair for independent mobility but do not wish to pursue a power wheelchair?
- Do you have an inefficient propulsion technique that's inhibiting your full participation?
If you answered yes to any of the above questions consider trialing a power assist device.
Check back next week as we continue our series on power assist devices.
References:
World Health Organization. (2001). International classification of functioning, disability and health: ICF. Geneva: World Health Organization.
 Angela Regier, OTD, OTR/L, ATP/SMS
Angela Regier, OTD, OTR/L, ATP/SMS
Clinical Education Manager ‑ Western Region
Angela Regier, OTD, OTR/L, ATP received her doctorate of occupational therapy from Creighton University in 2007 and is a RESNA-certified assistive technology professional. Regier joined Permobil in 2017 as a Clinical Education Manager for the western region. Prior to joining Permobil, Regier was at Craig Hospital in Englewood, Colorado where her career focused on inpatient and outpatient spinal cord injury rehabilitation. Prior to leaving Craig Hospital, she was supervisor of the Wheelchair Seating and Mobility Clinic where she provided comprehensive seating and mobility interventions for individuals with acquired brain and spinal cord injury. Regier has published and speaks on the topic of seating and mobility for acquired brain injury and spinal cord injury. She has also served as an adjunct faculty for the Creighton University Entry-Level Distance OTD Program (Regis) in Denver, Colorado.

 Curtis A. Merring, ORT, MOT
Curtis A. Merring, ORT, MOTDirector of Market Development, Manual Products
Curtis A. Merring, OTR, MOT received both his undergraduate psychology degree and masters in occupational therapy at the University of Pittsburgh. While at university he was involved in research on multiple studies dealing with psychosocial disorders, wheelchair seating, and neurological recovery of the upper extremity for stroke patients. As an occupational therapist and researcher for the past 9 years he was responsible for treating and investigating spinal cord injury and stroke. This included being awarded multiple small grants and coordinating research projects between the clinic and local universities. Curtis has also worked as a Director of Therapy Services in the geriatric setting including opening and managing rehabilitation departments at multiple locations. During his time as a director he developed a program called “Seating System Management in Skilled Nursing Facilities and Long Term Care”, that was a continuing education course he taught to facilities in both Texas and California. The goal of the course was to improve the seating systems of a very underserved population. Curtis is currently the Director of Market Development, Manual Products.

