For wheelchair users, maintaining skin health is a critical concern. The Clinical Practice Guidelines (CPG) emphasize that immobility is the primary factor associated with the risk of pressure injuries. Since wheelchair users experience prolonged pressure on specific areas of their body, they are automatically at higher risk. However, additional factors, including chronic disease and the natural aging process, further compromise skin integrity, making pressure injuries even more likely.
How Do Disease and Aging Affect Skin Integrity?
Chronic diseases such as Insulin-Dependent Diabetes Mellitus (IDDM) and vascular insufficiencies directly impact skin integrity. Additionally, the aging process naturally weakens the skin, making it less resilient to external forces such as pressure, friction, and shear.
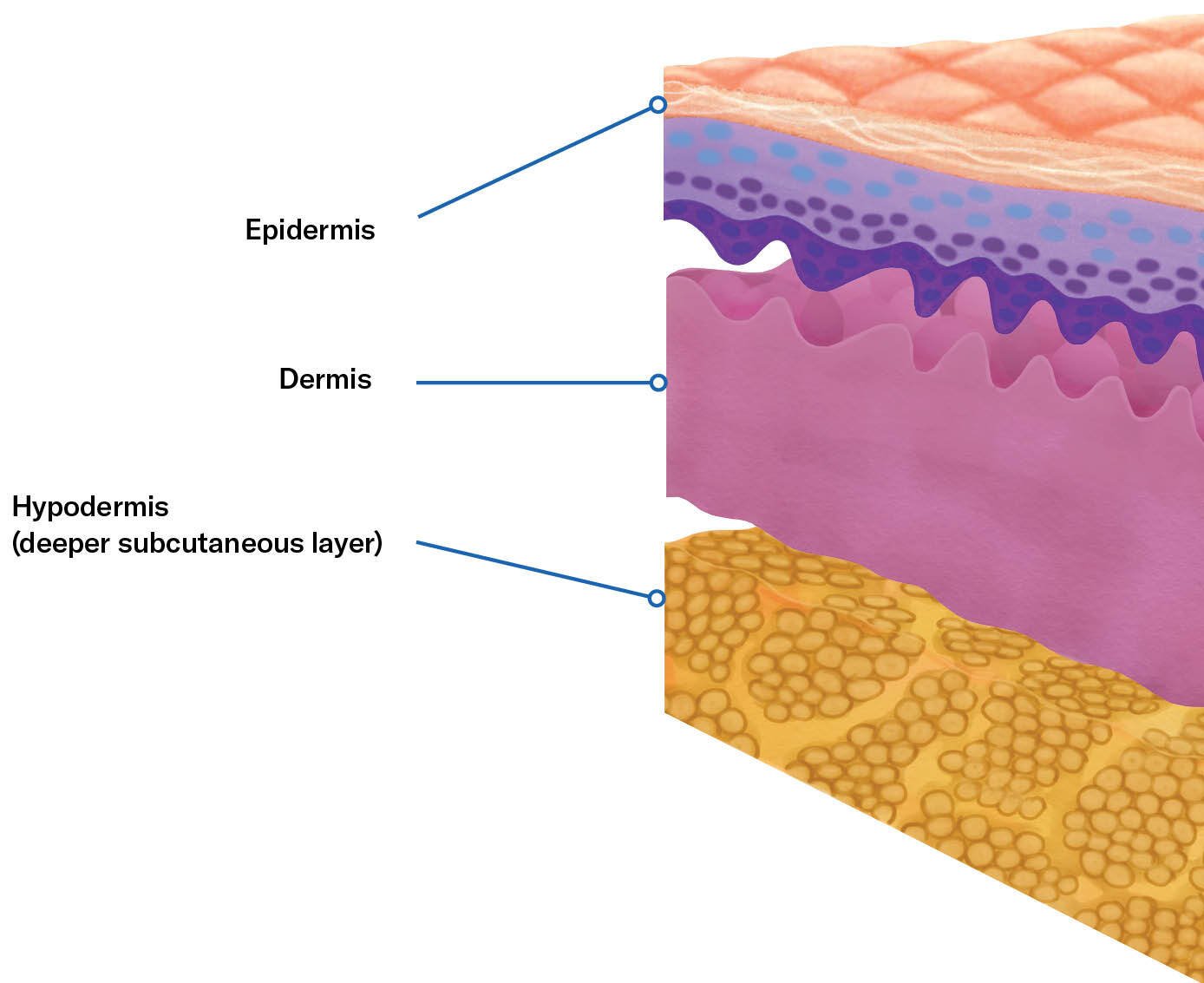
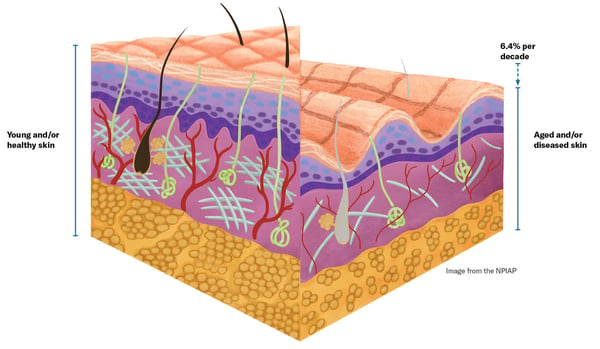
Every layer of the skin is affected by disease and aging, leading to a greater susceptibility to pressure injuries. Some of the most significant changes include:
-
Decreased Skin Thickness – The overall thickness of the skin diminishes, making it more fragile.
-
Reduced Sebaceous and Sweat Glands – These glands help maintain skin hydration and resilience; their decline leads to drier, more brittle skin.
-
Decreased Vascularization – Reduced blood flow means oxygen and nutrients are not transported as efficiently, which slows healing and weakens skin defenses.
-
Disorganized Collagen and Elastin Fibers – These structural proteins lose their integrity, reducing the skin’s ability to withstand mechanical forces.
-
Loss of Langerhans Cells – These immune cells help protect against infection and inflammation; their loss weakens skin defenses.
-
Flattening of the Dermal-Epidermal Junction – This structural change makes the skin more prone to damage from shear forces.
-
Diminished Nerve Endings – Reduced sensory perception can prevent individuals from detecting early warning signs of pressure injuries.
-
Fat Redistribution and Hypodermis Connective Tissue Loss – This results in less cushioning to absorb pressure, increasing vulnerability.
The Impact of These Changes on Pressure Injury Risk
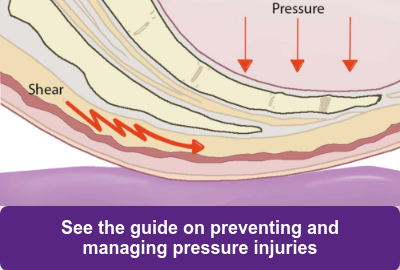
As these structural and functional changes take place, the skin becomes significantly more susceptible to damage from prolonged pressure, shear, and microclimate effects (such as excessive moisture or temperature fluctuations). Specifically:
- Oxygen and nutrients are not transported as efficiently, impairing healing.
- The skin becomes thinner, drier, and more brittle.
- Protective barriers diminish, increasing susceptibility to injury.
- The skin loses its natural resiliency, making it more prone to breakdown.
- Thermal regulation becomes impaired, increasing risk of moisture-related damage.
- Pain sensors become dulled, reducing awareness of early-stage pressure injuries.
The Challenge of Healing Compromised Skin
Once a pressure injury occurs, healing becomes far more challenging for individuals with compromised skin. The reduced ability to regenerate healthy tissue, combined with diminished blood flow and immune function, makes wound care a complex and prolonged process. Prevention is key—maintaining proper skin care, using pressure-relieving surfaces, and regularly shifting positions can help reduce the risk of pressure injuries.
By understanding these risks, wheelchair users and caregivers can take proactive steps to protect skin health and prevent potentially serious complications.
Want to learn more about pressure management and the prevention of pressure injuries? See our comprehensive digital Pressure Management Guide.
Commercial Product Manager - Permobil Americas
Nicole B. LaBerge, PT, ATP is a Physical Therapist with 18 years of experience in a variety of clinical settings. She currently works for Permobil as a Commercial Product Manager of Seating and Positioning products. Her past clinical practice has included seating and mobility for adult and pediatric populations, with a focus in neurological rehabilitation, power standing and wound care. Nicole has presented at the State and International Levels, has multiple publications in peer reviewed journals and enjoys sharing her passion for patient advocacy, efficiency, and clinical outcomes. She served as an Executive Board Member for the Clinician Task Force for 3 years and is currently an active member in the CTF.