Update your browser to view this website correctly. View list of available browsers
This guide is intended to help equip therapists to make the most appropriate mobility recommendations for their clients and will increase their confidence and knowledge of power mobility.
Wheeled mobility options can be overwhelming, and it's important to understand when it is clinically appropriate to move to power mobility. This guide is intended to help therapists: Understanding the qualifications for both manual and power wheelchairs
Our hope is that this guide will equip therapists to make the most appropriate mobility recommendations for their clients and will increase their confidence and knowledge of power mobility.
This guide is meant to be a comprehensive introduction to power mobility. For advanced learning opportunities, visit the education tab at permobilus.com
This guide is not intended to replace the advice of a medical professional. This guide was created using process and funding guidelines for the United States, including Medicare terminology.
To download the Power Wheelchair Guide as a PDF click here.
Look for these info boxes throughout the guide. They include quick tips or takeaways for that section.
A variety of factors must be considered when determining if powered mobility is the appropriate solution for your client.
Start with the client and their unique medical, functional, and environmental needs. The following are some considerations to get you started. There are likely other factors that apply to your specific scenario as well. Just remember, the goal is safe and efficient mobility in all necessary environments!

Chapter 1
Our guide to Wheeled Mobility 101 goes over the basics of DME and CRT equipment from understanding DME & CRT equipment to determining if your client is an appropriate user for DME or CRT equipment. Check out that information here.
Once you've identified the need for wheeled mobility for your patient, you must consider their need for power mobility. If they are unable to FUNCTIONALLY propel an optimally configured manual wheelchair, then power mobility needs to be considered.
Remember that "functionally propel" includes the ability to propel in all the desired environments in a safe and efficient way
Consider a client's prognosis and what their needs will be in the future. For example, a person with newly diagnosed ALS may still be able to perform independent pressure relief, but will need power tilt and recline in the future as the disease progresses
An individual must have the cognitive ability to drive a power wheelchair
An individual must express wanting to use a power wheelchair
Always schedule a power wheelchair trial if you question your client's cognitive capacity to drive. Technology exists that allows people of varying abilities to drive and control a power wheelchair.
All of the basic criteria for a manual wheelchair apply AND they must meet the basic power wheelchair criteria below:
1. They are unable to propel an optimally configured manual wheelchair due to upper extremity limitations:2. The home has adequate access for maneuvering of the power wheelchair
3.Use of the power wheelchair will significantly improve their ability to perform MRADLs
Click on each standard power wheelchair option below to learn more
Standard power wheelchair options |
|||||
| Limited adjustability | Most customizable | ||||
| Scooter | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 |
| DME | CRT | ||||
CRT equipment requires a physician face-to-face appointment, an OT/PT evaluation, and an ATP directly involved in the equipment choice.
Chapter 2

As indicated in the chart of Standard power wheelchair options, DME power mobility devices usually have limited adjustability. The following DME products meet all of the basic power wheelchair criteria while having their own qualifying criteria. Click on each category to learn more about the qualifying criteria and limitation of each DME power mobility device.

As indicated in the chart of Standard power wheelchair options, CRT power mobility devices are the most customizable power mobility devices. The following CRT products meet all of the basic power wheelchair criteria while having their own qualifying criteria. Click on each category to learn more about the qualifying criteria and limitation of each CRT power mobility device.

The drive wheel on a power wheelchair is the larger wheel if you are looking at the wheelchair.

The location of this drive wheel can have a large impact on how the power wheelchair drives and maneuvers in different environments.
When determining drive wheel placement always consider the primary environments the wheelchair will be used in as well as what the client has used previously, if not their first wheelchair.
Changing the base type is not a decision that should be taken lightly! The client’s entire motor memory is wrapped into the specific drive wheel they are used to using, their environment, and modified vehicle may also be set-up to accommodate this configuration. The client should be educated on what the change in drive wheel configuration will mean from a learning curve and adjustment period standpoint.
For indoor use, consider the turn radius/maneuverability. This is very important to many users as it will dictate the ease of entry into rooms and how close they can get to surfaces in order to perform an MRADL.
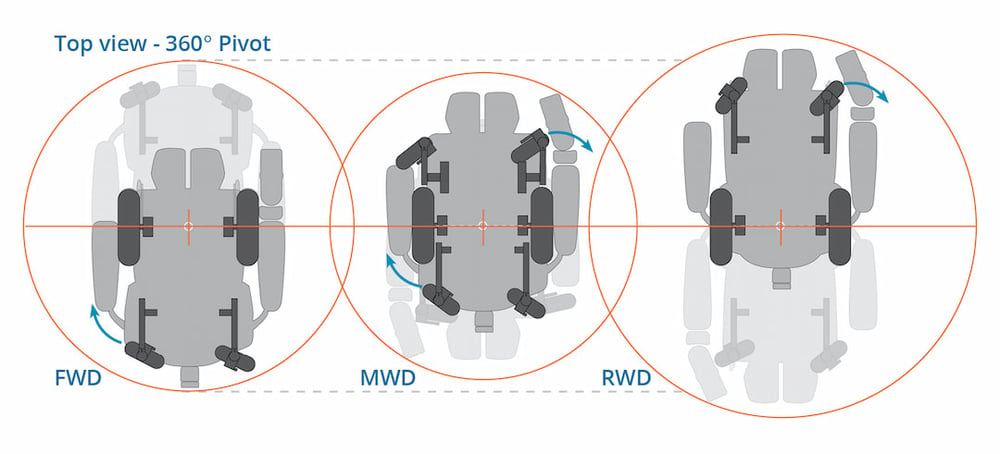
Base length, including the footrests plus the drive wheel position, will determine the turning radius. Keep in mind that a turning radius does not equate to functional maneuverability.
People have a tendency to steer clear of front wheel drive because:
Both of those statements may be true depending on the person (some people feel FWD is easier to learn), BUT NOT A REASON TO STAY AWAY!
Front wheel drive may be less intuitive to learn how to drive versus mid-wheel drive, but with a little practice and a few key tips, many users have success in learning to drive a FWD base.
The two key points when teaching to drive a front-wheel drive wheelchair is:
1. Hug the corner. When going through a doorway the end-user will want to “hug” the corner or keep a tight turn.
2. Turn towards the problem. For example, when positioned adjacent to a wall/barrier, turn toward the wall/barrier, then slightly reverse to allow the rear casters clearance for turning in the desired direction. This might sound complicated, but if you remember to turn into the problem you will easily maneuver away from the problem.
Some users find FWD the easiest to learn as it feels most like walking when taking turns. When walking, we typically initiate turning into a doorway as soon as we get to the corner vs. walking to the center of the door, then pivoting.
Power seat functions are simply the different positions that a power wheelchair can achieve by using a joystick, alternative drive control, external switch, or switch box. Click on each power seat function below to learn specifics. 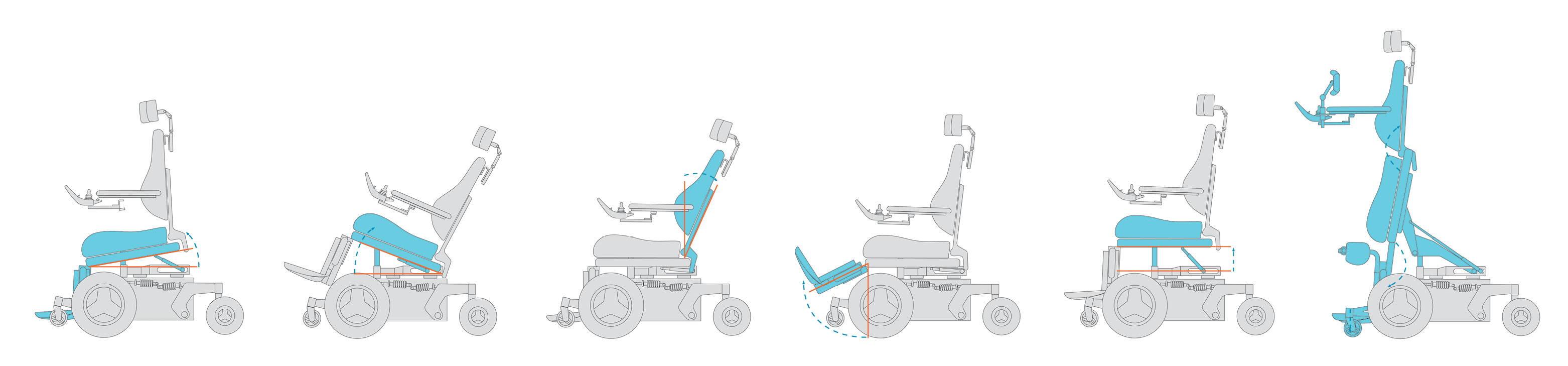
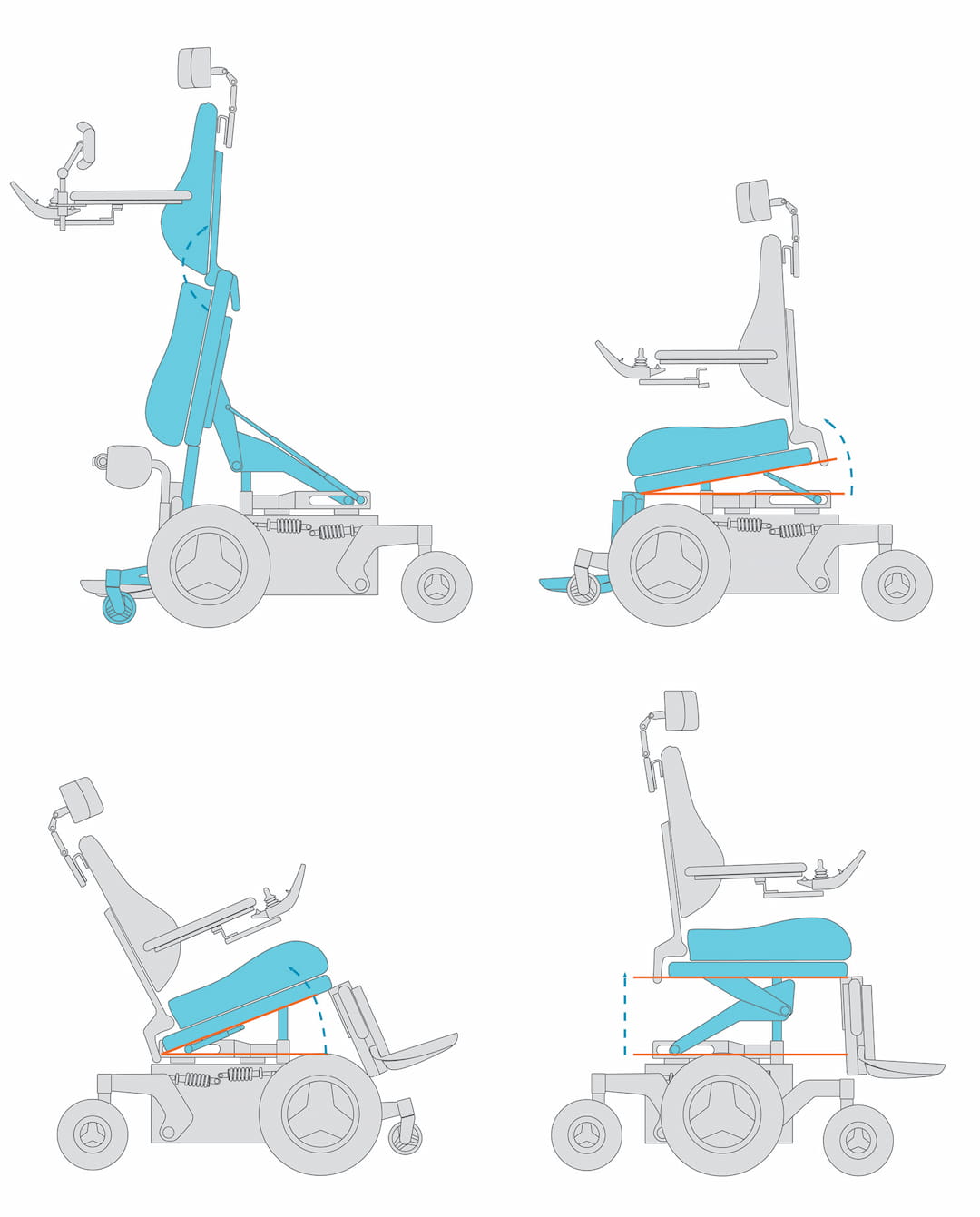
Power tilt can refer to anterior tilt where the seat tilt anteriorly "without changing the seat-to-back angle" (Waugh & Crane, 2013, p. 48) or to posterior tilt where the seat tilts "posteriorly without changing the seat-to-back support angle or seat to lower leg support angle" (Waugh & Crane, 2013, p. 48)
Power recline "allows the back support to pivot posteriorly, increasing the seat to back support angle" (Waugh & Crane, 2013, p. 48)
Allow clients to change the seat to lower leg support angle in order to flex or extend the knee.
Some legrests articulate, that is, lengthen while extending the knee.
Power seat elevation "allows raising and lowering the whole seating system, changing the seat to floor height without altering the angular orientation of the seating supports" (Waugh & Crane, 2014, p. 48)
Power standing "is capable of raising the occupant from a seated to a standing position by changing the orientation in space of all the primary seating support surfaces" (Waugh & Crane, 2013, p. 48)
Power seat functions can always be combined. The available power seating options, however, are dependent to some extent on the type of power wheelchair base selected. Not all power wheelchairs can accommodate all power seat functions or the amount of the power seat function required for medical and/or functional needs.
There are two different style of drive control: proportional drive control and non-proportional drive control.
Proportional drive control means that the driving action (speed, direction) is relative to the amount of deflection of the joystick away from neutral and the direction of that deflection. A proportional drive control can be a standard joystick, or it can be a variety of other alternative drive controls that have similar functionality.

Benefits may include |
Considerations |
|
Infinite control of speed based on amount of user input |
Most require some amount of range of motion and strength to activate, this may not be possible for everyone |
|
360° of directional movement |
For someone with severe cognitive impairment, the freedom of movement of the drive control may be too demanding and may do better with an “on”/”off” non-proportional drive control |
|
Continuous fluid response of wheelchair as the user moves the drive control away from neutral |

When considering a proportional drive control, you must consider the client’s movement and strength as it relates to the throw and force required of the drive control.
Throw: The amount of deflection or travel (from neutral) it takes to reach maximum speed (typically measured in millimeters)
Force: Force required to move the joystick from neutral (typically measured in grams)
Other programming considerations include:
• Drive parameters – acceleration, deceleration, speeds
• Sensitivity/Tremor dampening
• Deadband: the “neutral zone”, the deadband setting is the amount of joystick deflection from neutral required before driving commences
• Changing axis if needed: the ability to change the joystick direction configuration
When an individual does not have the strength, range of motion, and/or coordination to operate a proportional drive control, a non-proportional input device may be considered.
Also known as switched or digital drive control, these devices are either “on” or “off” and typically allow 4 to 8 discreet directions of movement.
For example, the wheelchair may be controlled by four individual switches that the user hits to activate the wheelchair – one for each direction of forward, reverse, left, and right.

A six or eight direction control might have a command or switch for each of the following directions.

|
Key phrases for non-proportional drive controls |
|
|
Momentary |
A switch must be continuously pressed (or activated) in order for the power wheelchair to drive. When the switch is released, the chair will stop driving |
|
Latched |
A single press (or activation) of the switch will activate the power wheelchair in that direction for a specified period of time or until the user gives an input for the chair to stop |
|
Mechanical switch |
The user must apply a force to the switch to displace it and thus activate the desired function (switches with different force/travel requirements are available depending on the user’s strength and range of motion) |
|
Proximity switch |
A proximity switch is a type of electronic switch that does not require any force to activate. The user must simply come within a specified distance of the switch to activate |
|
Fiber optic switch |
A fiber optic switch is a type of electronic switch that does not require any force to activate. The user must either maintain or break a beam of light to activate |
|
Pneumatic switch |
A pneumatic switch is a type of switch that is activated by changes in air pressure |
Programming considerations
The are key factors when evaluating power base performance. Power wheelchair bases should be able to help a user navigate a variety of spaces and terrain safely and efficiently. Suspension, torque, and tracking all play a key factor in the wheelchair's ability to do so with minimal jarring to the user.
"Mechanism of a device that is intended to reduce vibration" (Waugh & Crane, 2013, p. 32)
Torque is the twisting/turning force that causes rotation around an axis. In power wheelchairs this is a function of appropriate gearing of the gear box to assure the powerbase can navigate obstacles effectively.
“Motor technology that helps a power wheelchair to travel in a true forward direction on various terrains” (Waugh & Crane, 2013, p. 43).In short, tracking technology helps the wheelchair stay on the desired route by compensating for environmental aspects that would otherwise cause the chair to veer.
Chapter 3
Our beginner's guide to fundamentals of wheeled mobility, Wheeled Mobility 101, goes over the therapy evaluation along with how to measure for properly fitting wheelchair components. Click on the links below to learn more about each topic.
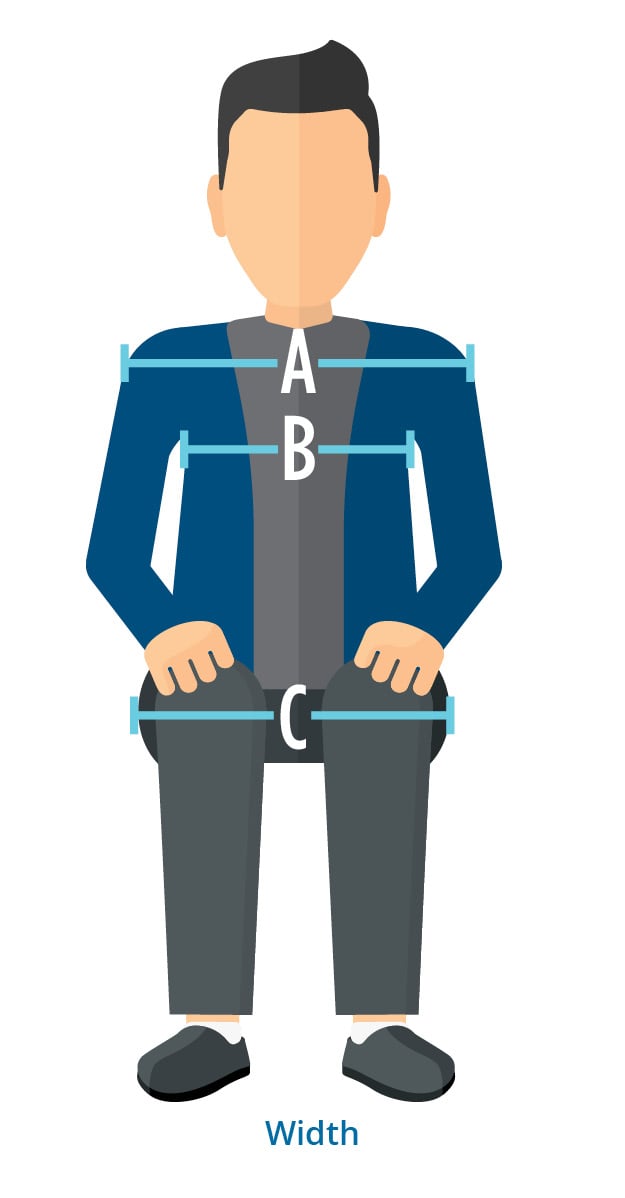
How to measure shoulder width (A):
Measure from humeral head to humeral head, incorporating excess tissue
How to measure chest width (B):
Measure from axilla to axilla, this measurement helps determine back support width
* These measurements will determine the width of the back support, and the distance placement of laterals if applicable.
How to measure Hip width (C):
Measure from widest point to widest point of the hips, including all residual tissue
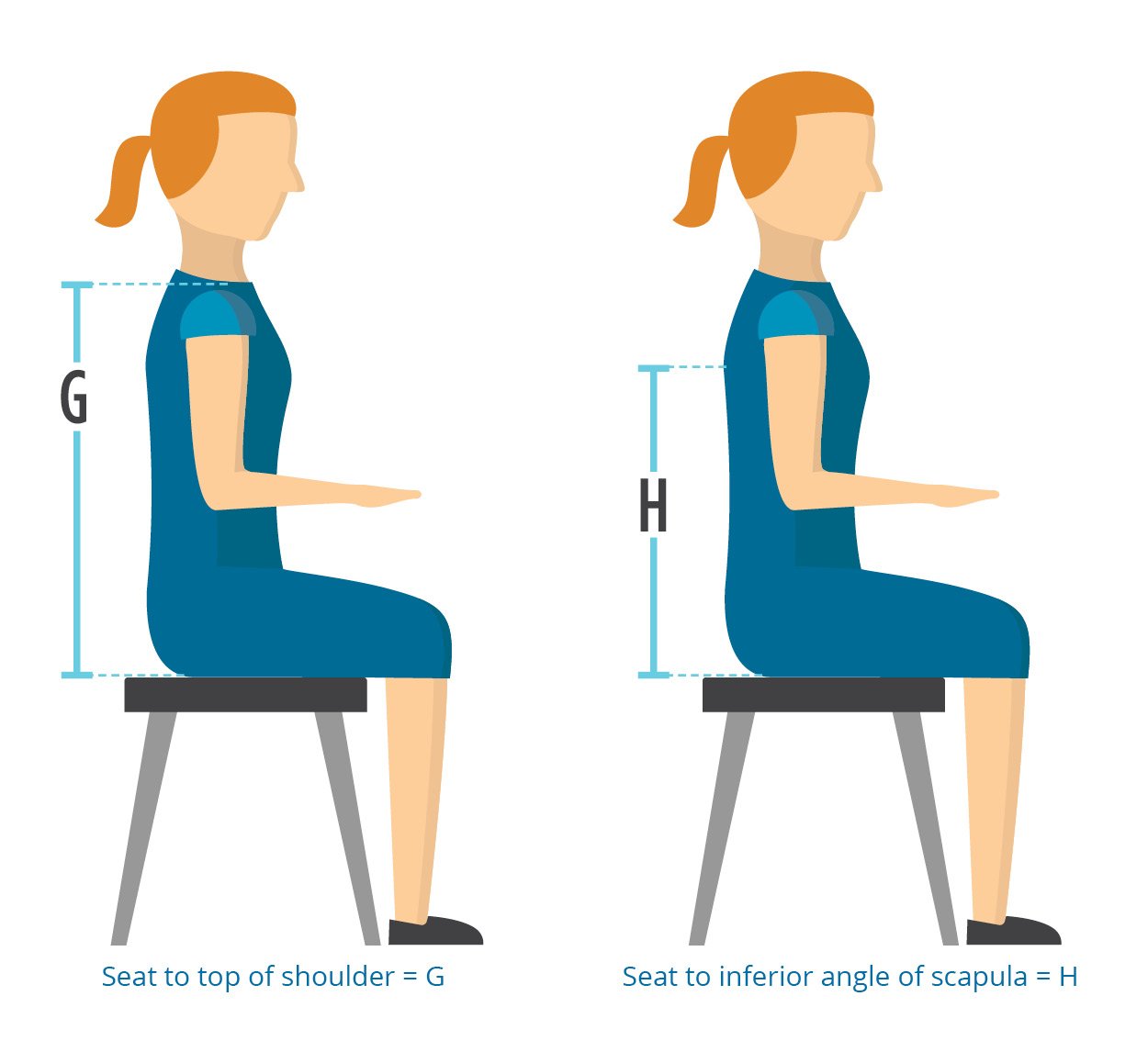
How to measure (g or H):
Measure the patient in the position you are striving to achieve
* These measurements will help you determine the length of the back support. Consider whether the back support height can be adjusted on the power wheelchair when determining length.
* Back support length= The measurement of the back support itself
Back Support height= The height of where the back support is placed on the power wheelchair
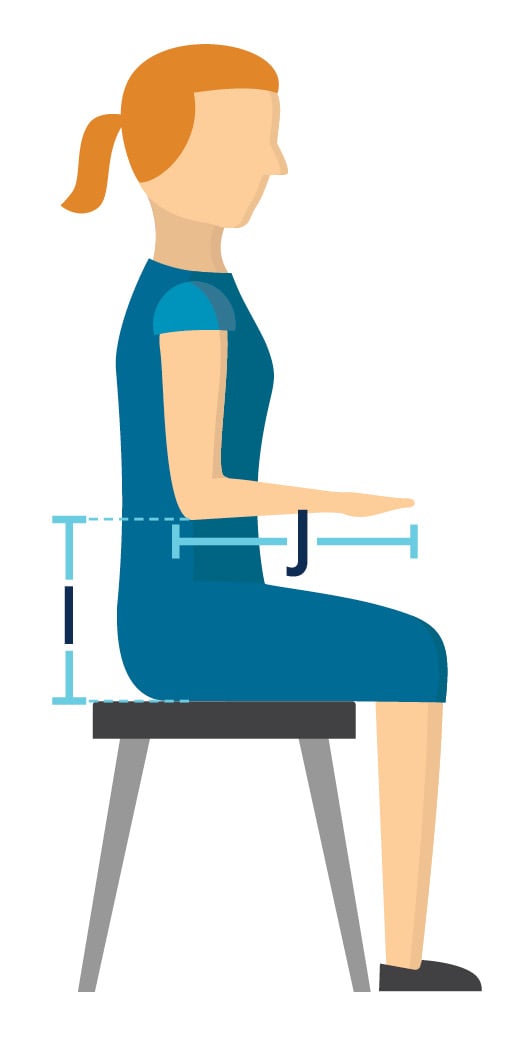
How to measure seat to elbow height (i):
Seat your client with shoulder in neutral and elbow bent at his or her side to 90°
Measure from top of seat to under forearm/elbow
* Measure both sides in case of a non-reducible pelvic obliquity/scoliosis. These measurements will determine the length of the arm support and the height it should be placed.
How to measure Forearm length (j):
If patient needs a specialized arm length, measure from end of elbow to where the therapist wants the desired replacement arm support to end

How to measure UPPER leg length (K):
Measure from the back of the buttock area, including all excess tissue, along the femur to the popliteal fossa.
How to measure lower leg length (L):
Measure from popliteal fossa to bottom of foot. If they normally wear shoes, include shoes with measurement.
* Upper leg length measurement will help guide the PWC seat depth ordered.
* Lower leg length measurement, when considered in conjunction with cushion selection, helps determine the placement of the footplates on the power wheelchair.
Some Group 2 bases will allow this, but it is most common in Group 3 and above.
CRT seating components:
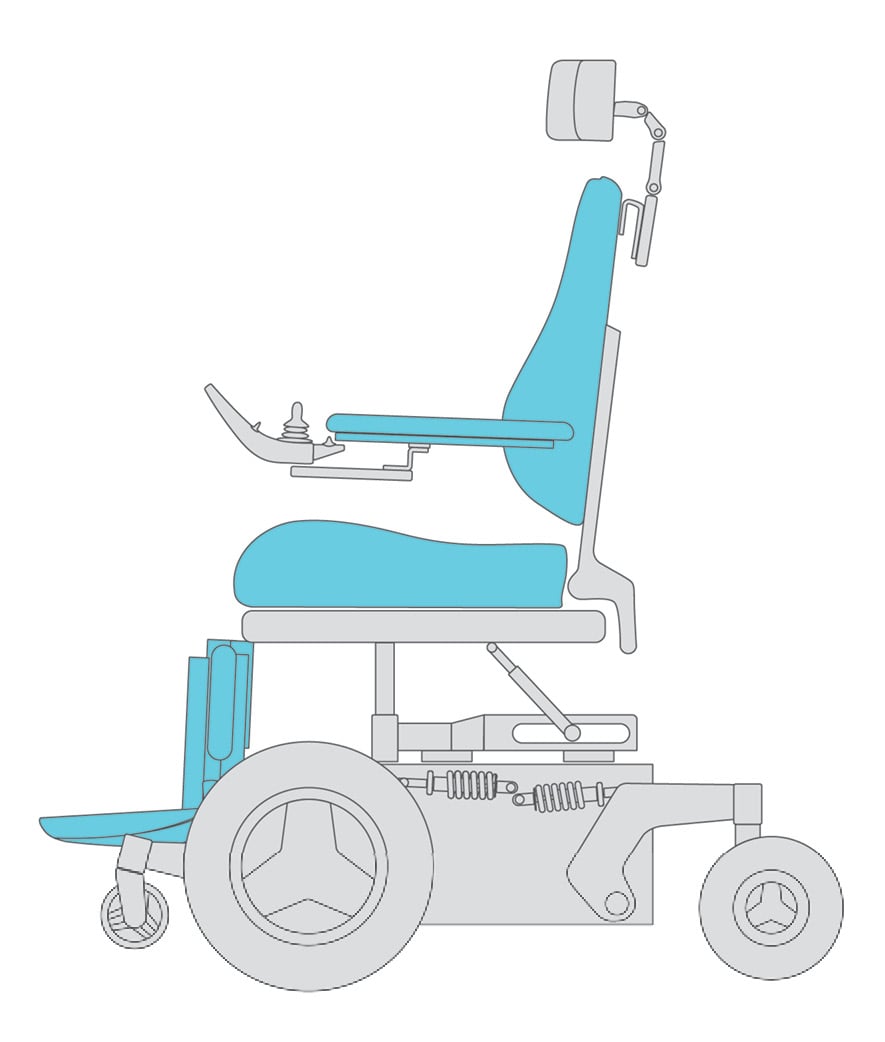
Primary support surfaces are the primary weight bearing surfaces when seated in the wheelchair and include:
It’s important to select appropriate primary support surfaces to maximize postural alignment, skin protection, and function.
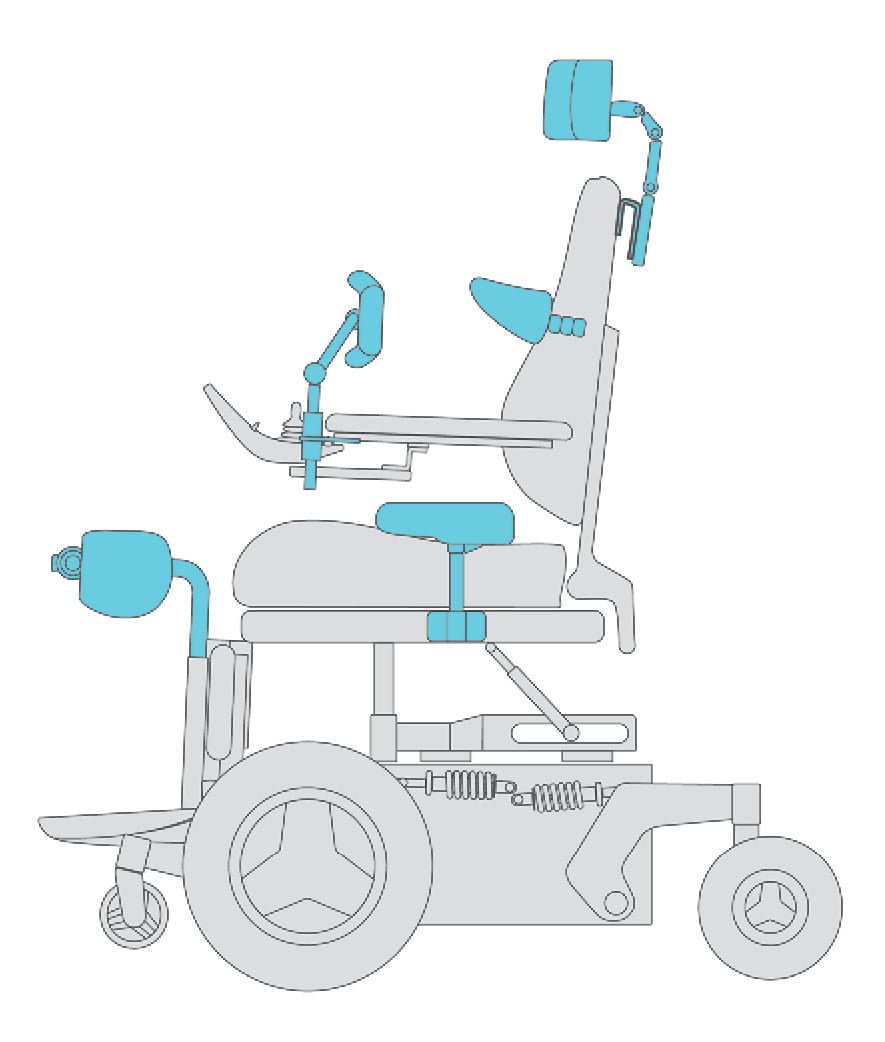
Secondary support surfaces are the other support surfaces of the seating system and may include:
Secondary support surfaces may be required to optimize support, postural alignment, skin protection and function for individuals with limited motor control and/or postural asymmetry.

Chapter 4
NO. Funding is highly determined by the functional and medical needs of a client. Although Medicare states “the beneficiary’s mobility limitations is due to a neurological condition, myopathy or congenital skeletal deformity”, a clear picture of functional and medical reasons can justify the need for power mobility.
There is no cookie cutter solution for funding powered mobility devices. Every individual is unique and has specific needs and therefore best practice is to always put the client first!
Often a “top down” model is used with the funding source (i.e., insurance) at the top deciding what is and isn’t paid for. Unfortunately, at times, this leaves the consumer as the last to be considered in the equation.
For example, under Medicare, a seat elevator is considered a luxury item and not deemed medically necessary even though this power seat function could mean the difference between independence or the need for assistance with a transfer.
This approach has a trickle-down effect on client access and product innovation. If a function or item improves independence, it should be medically necessary and paid for by the funding source.
Client needs should drive funding, not the other way around!
Yes! Permobil offers an on-line LMN Generator.
For free access to template justification language, sign up at www.permobillmn.com. Templates are a great starting point, but your justification must always be customized to the individual client and their specific medical and functional needs.
For client’s with complex needs, a Group 2 base may not provide the necessary features resulting in sub-optimal outcomes. Specifically:
While a Group 4 power mobility base is considered a non-covered item under Medicare, some state Medicaid and private insurances will cover a Group 4 base with the appropriate justification. Remember, recommend what your client needs medically and functionally!
In addition, Group 4 power mobility bases are not just for outdoor use. You may consider a Group 4 base for other reasons such as:
Power seat elevation is covered by some state Medicaid programs and private insurances. Use of vocational rehabilitation funds may be a consideration as well if the person is attending school or work, and the seat elevator helps them in those roles.
The following five questions are frequently asked in the industry. Click on each question below to find out the answer.
Chapter 5

There are a few topics in power mobility that are not easily classified into a category. In this section we explore these topics of special consideration.
Children develop through movement.
Play is how babies/toddlers interact with their environment and is a vital activity in all aspects of development. (Rosen, L et al 2017)
Children with cognitive and/or physical limitations respond to play as well, and when provided with the ability to move, can even initiate play with others. Early power mobility can provide a child the opportunity to play and interact rather than simply being an observer.
Just like babies/toddlers need to learn the skills of rolling over, crawling, and walking, young children need to learn the skills for power mobility. Children as young as 14-17 months old have shown the ability to learn power mobility skills when provided with frequent opportunities to practice. (Casey, et al 2013)
Remember they may struggle and fail just like toddlers fall frequently when learning to walk. But by providing encouragement and repeated opportunities to learn, a young child can learn to use power mobility to play and explore his environment.
|
Benefits may include |
Considerations |
|
Depending on the size of the child, the power wheelchair may have a smaller footprint and turning radius than a manual wheelchair. |
If a child is going to ride in the wheelchair in a vehicle, there needs to be access, tie downs, and compliance to safety regulations |
|
Multiple seating and positioning options can promote postural stability and minimize the development or progression of abnormal postures or pressure injuries |
If a child will ride in a car seat, most power wheelchairs will require a lift to transport the wheelchair |
|
Certain power wheelchair options allow for a child to rest and be toileted in their chair without the need to be transferred to the bed |
|
|
There are multiple ways to access and control a power wheelchair |
|
|
Power wheelchairs can be paid for by insurance if a child meets the requirements. This can vary greatly in different parts of the country and your supplier can help you navigate the process. |
No. At this young age, a PMD is used as a therapeutic tool for short periods while supervised. It creates opportunities for toddlers to develop strength, exploratory behaviors, emotional expression, and postural control. (Plummer et al., 2020)
Self-initiated movement is critical to promoting developmental milestones. A PMD allows for on-time mobility during this crucial period of development.

A power assist is the use of technology to assist with the "push" phase of independent manual wheelchair propulsion. Learn more about power assist devices in our manual wheelchair guide.
Be proactive instead of reactive! Power assist can prevent upper extremity overuse injury and promote increased independence and safety.
I can’t provide power assist because a Group 2 power wheelchair is so much cheaper. Is this true?
Insurance companies typically pay for the least costly, medically appropriate alternative. Here are some considerations to determine when power assist may be most medically appropriate:
Although a Group 2 power wheelchair is more cost-effective, it offers limited positioning options and a footprint that may not fit well in some environments. Always consider the client’s environment and daily activities.

It’s using a different way to drive the wheelchair and access your power seat functions. Joysticks are the standard, but sometimes clients don’t have the upper extremity control, endurance, or coordination to use a joystick.
What if my client can't use a standard joystick?
Address the following with a standard joystick before changing to an alternative drive control:
Once you've assessed all the considerations on page x with a standard joystick an alternative drive control may be required:
Often the mounting of the drive control is as critical as the drive control itself!
Click on the different types of alternative drive controls to learn more about each
Uses head movement to activate proximity or mechanical switches built into pads. Some newer models also have a proportional component.
Sip & puff is a pneumatic switch that uses varying air pressure from the person's mouth via sips in or puffs out, to control the wheelchair.
A switch array is a series of two or four switches (proximity or fiber optic), typically mounted in a tray, used to operate the power wheelchair. Multiple switches can also be set-up wherever needed based on the user’s available movement. When using multiple switches, a combination of mechanical, proximity, or fiber optic switches may be used based on the available movement and strength at each switch site.
Single switch scanning allows for operation of the power wheelchair with a single switch. The user display (or separate box mounted to chair) gives a visual cue of direction (example pictured below), typically through an arrow or light that scans 4 to 8 discreet directions. The user activates the switch once the arrow or light reaches the desired direction. The switch may be programmed as momentary or latched.
Eye gaze allows for power wheelchair operation through use of eye movement via an eye tracking device and tablet computer mounted on the wheelchair.
Wheelchairs have advanced with technology in recent years, and these features can help your clients in many ways.
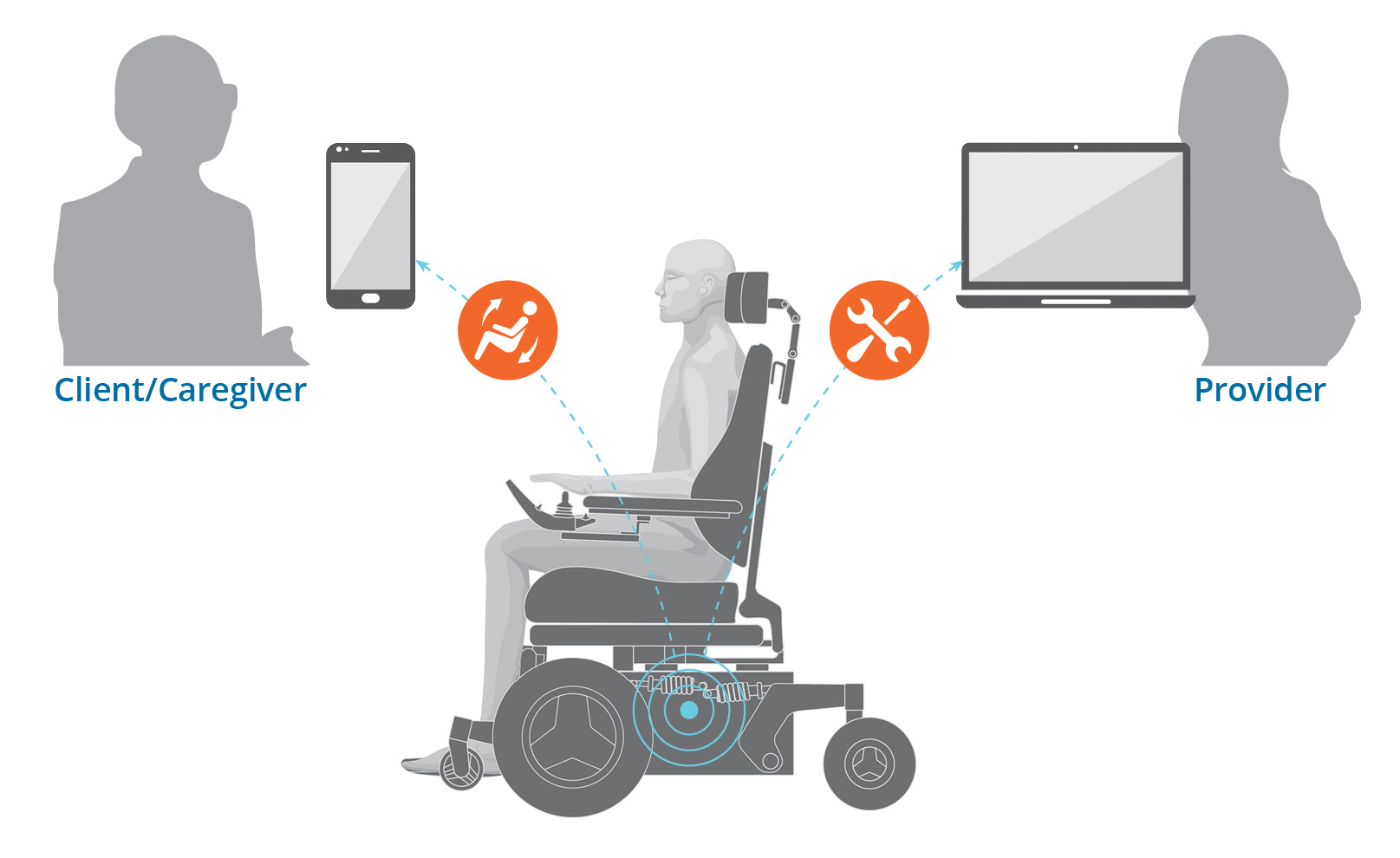
Bluetooth: Advanced electronics allow end users to connect to their smart devices via Bluetooth technology. This enables them to use the input device to both drive their wheelchair and control their paired phone or tablet.
Apps: Some manufacturers have developed wheelchairs that communicate with apps on their smart devices. These can provide end users with:
Remote connectivity: Service technicians can remotely access wheelchair data to help diagnose potential issues, resolve simple fault codes, and better prepare for service visits.

It's important to keep the following in mind as you work through the evaluation, justification, and delivery process. Think about both short and long-term needs, and then do the best you can for your client! Evaluate each individual to identify their needs and goals medically, posturally, functionally, and environmentally.
Maximizing client comfort, minimizing pain, correcting deformities when possible, preventing further deformity, preventing pressure injury, maximizing safety and functional independence, assuring independence in all necessary environments.
Identify seating and mobility equipment that will meet these needs. Connect clients needs to recommended equipment solutions in documentation.
Remember that power wheelchairs with power seat functions can provide important health, function and participation benefits - think big picture when evaluating how power seat functions may improve outcomes!
Power assist devices can be a great solution if a manual wheelchair base is most appropriate given the clients environmental and functional needs.
A client-centered evaluation and delivery, including set-up and training on the device, are key to success in achieving best client outcomes.
You are going to need to advocate for your patient now in order to get them the proper equipment that can address their needs over time.
Click here to download the Power Wheelchair Guide as a PDF.
Click here to view the glossary for the guide.
Click here to view the list of references.
Remember, there are no "standard" solutions when providing power wheelchair mobility. Each client is unique and deserves a system that is tailored to their individual needs and goals. Just use your clinical reasoning skills to figure out what's best within the given parameters.

For more information click here to contact your local representative
The Power Wheelchair Guide is available for download. Click here to get your PDF copy.
All contents © copyright 2019 Permobil. All rights reserved.
Sign up for email notifications
1. Lisa K. Kenyon, Maria Jones, Becky Breaux, Jessica Tsotsoros, Tonya Gardner & Roslyn Livingstone (2019): American and Canadian therapists’ perspectives of age and cognitive skills for paediatric power mobility: a qualitative study, Disability and Rehabilitation: Assistive Technology, DOI: 10.1080/17483107.2019.1606858
2. Whitney, P. G., & Green, J. A. (2011). Changes in infants’ affect related to the onset of independent locomotion. Infant Behavior and Development, 34 (3), 459–466. https://doi.org/10.1016/j.infbeh.2011.05.001
3. Stavness, C., (2006). The effect of positioning for children with Cerebral Palsy on upper-extremity function: A review of the evidence. PT and OT in Pediatrics, 26,39-52)
4. Kenyon, L. K., Schmitt, J., Otieno, S., & Cohen, L. (2019). Providing paediatric power wheelchairs in the USA then and now: a survey of providers. Disability and Rehabilitation: Assistive Technology, 1-10. https://www.tandfonline.com/doi/abs/10.1080/17483107.2019.1617358?journalCode=iidt20