In the world of seating and mobility, pressure injuries are a big deal. It is our job as clinicians and therapists to prevent peak pressure through the use of seating and positioning products, to minimize risk of pressure injuries. In today’s blog we’re taking a look at the mechanics of pressure injuries and will identify some scenarios in which a wheelchair user could benefit from a short-term positioning surface to safely perform daily tasks.
The Mechanics of Pressure Injuries: It's Not Just Ischemia
Before we talk about the solutions, I’m going to speak first about the problem. As I’m sure you’ve heard before, ischemia was the most widely accepted and most researched cause of pressure injuries. Ischemia is a lack of blood flow. However, Stekelenburg, a well know pressure injury researcher, in 2007 performed a study* in animals refuting that a lack of blood flow is the primary factor in tissue necrosis. In that study, they looked at cell death with ischemia and compared it to cell death with ischemia and force loading or pressure. They found that more damage was caused by a combination of ischemia and tissue distortion vs ischemia by itself. This concept of sustained cellular deformation leading to cell death has become more well-known and increasingly researched mechanism of pressure injury ideology.
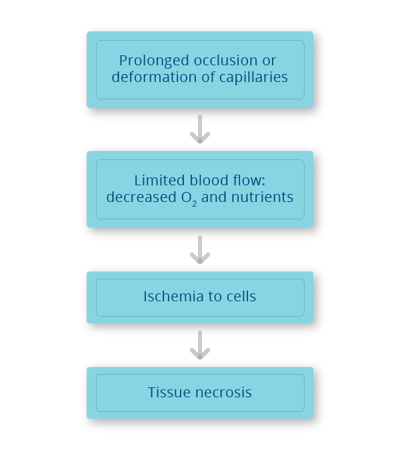
Simply put, under load large compressive and tensile strains induce large deformations at the cellular level. Large cellular deformations can stretch the plasma membrane of individual cells. This damage to the plasma membrane could disrupt cellular homeostasis and eventually cause cell death and result in tissue injury. Damage from deformation can occur not only at the organ and tissue level but also at the cellular level, and this damage can even occur in situations where there is good blood flow.
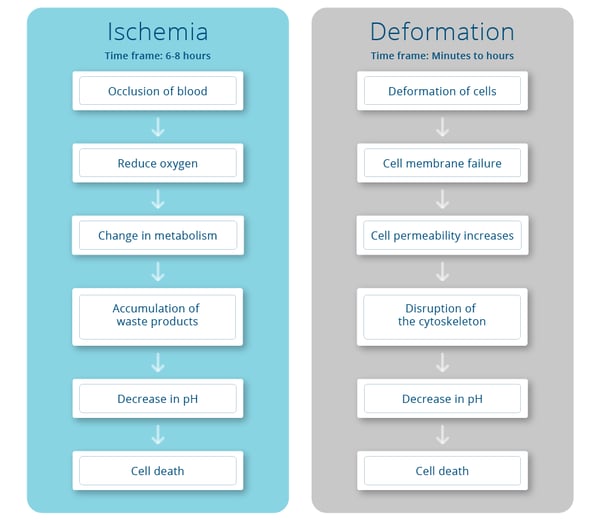
We are not just worried about blood flow and circulation; we are now also concerned with cellular deformation. The two charts here compare and contrast what happens during ischemia and cellular deformation, but the end result of each pressure injury pathway is still cell death. And more importantly the time frames are quite different. Considering cellular deformation can happen in minutes to hours, it’s extremely important to address the wheelchair users skin protection needs beyond the wheelchair. This includes surfaces they are sitting on for bathing, toileting, driving, and beyond.
Scenarios for Short-Term Seating Surfaces
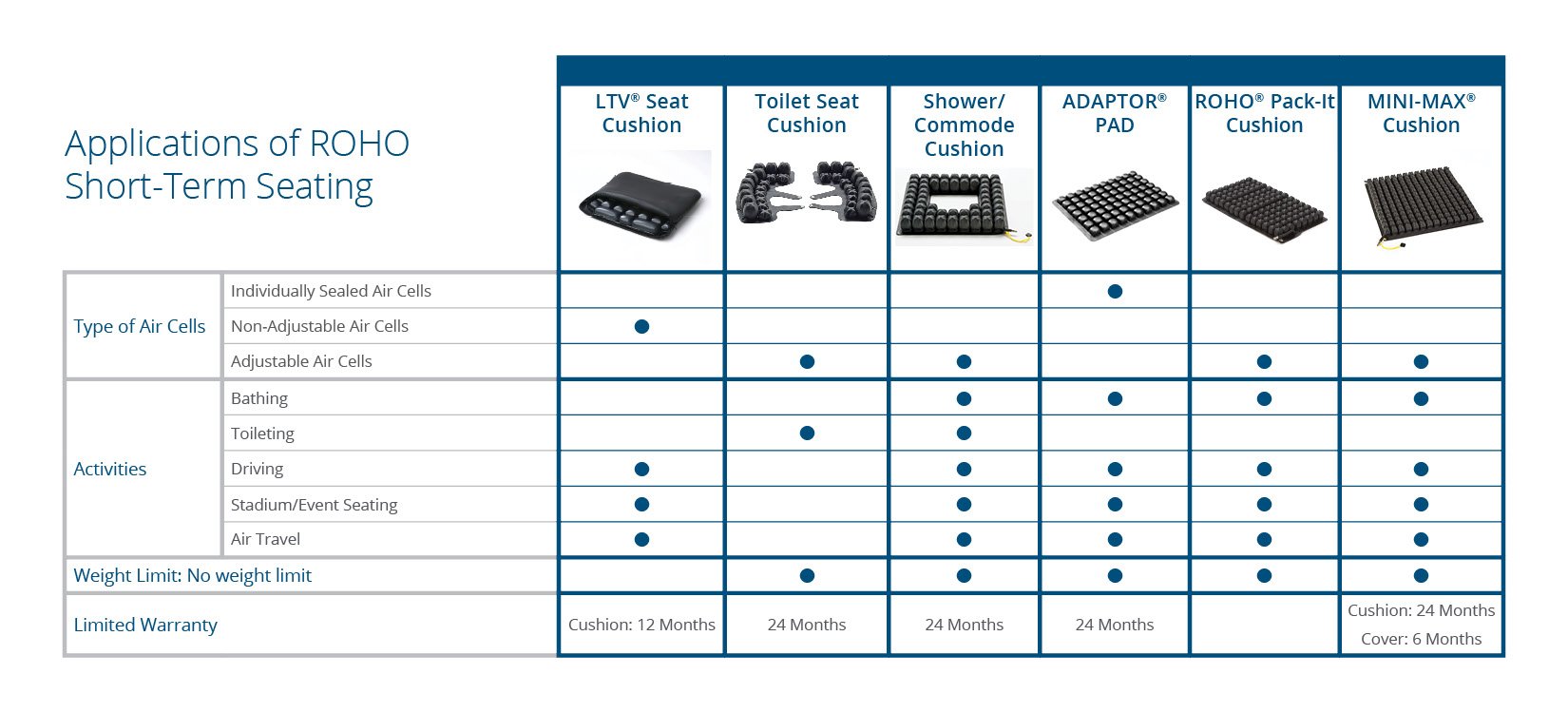
As we mentioned in the above paragraph, cellular deformation can happen in a matter of minutes. Taking this into consideration, our clients can minimize the risk of pressure injuries by using short-term seating solutions. Below is a chart of activities where ROHO short-term seating solutions can be utilized to minimize deformation, inflammation and ischemia in these scenarios.
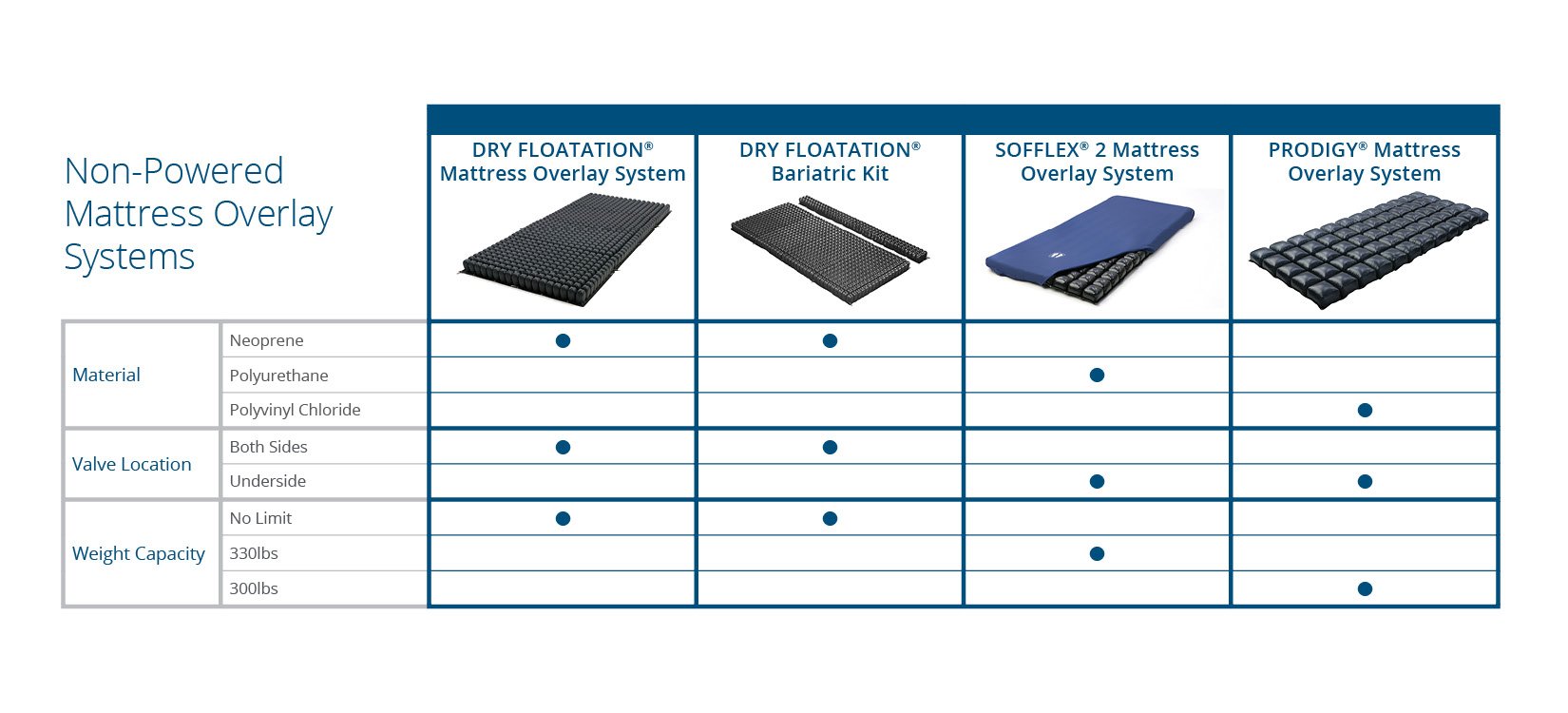
Skin protection in bed is vital. “Bed sores” have historically caused debilitating pressure injuries to wheelchair riders. Our clients rest and sleep in bed at least eight hours a day. ROHO has a line of mattresses and overlays which offer the skin protection many clients need while supine and in a reclined position. See the chart below for a description of the ROHO mattress line.
Given what we know about cellular deformation and pressure injuries we encourage clinicians assess and address the skin protection needs for MRADLs in bed, the bathroom, and beyond. These short-term seating surfaces, mattresses, and overlays can be ordered through suppliers and/or through eCommerce. This gives a variety of access methods to these products which can make a world of difference in protecting skin and optimally preventing skin breakdown. By making it common practice to select appropriate skin protection products for use outside of the wheelchair, we can further reduce pressure injuries for the at-risk client population.
*Stekelenburg, A., Strijkers, G. J., Parusel, H., Bader, D. L., Nicolay, K., & Oomens, C. W. (2007). Role of ischemia and deformation in the onset of compression-induced deep tissue injury: MRI-based studies in a rat model. Journal of Applied Physiology, 102(5), 2002-2011.
 Eleni H. Lema, MOT, OTR/L, ATP/SMS
Eleni H. Lema, MOT, OTR/L, ATP/SMS
Eleni Halkiotis Lema, MOT, OTR/L, ATP/SMS is a Regional Clinical Education Manager for Permobil supporting the New York City and mid-Atlantic areas, South Florida, and Latin America. Eleni joined Permobil in 2019 and prior to this worked in wheelchair clinics in New York City including Independence Care System and Bellevue Hospital. Eleni has presented professionally in the USA and internationally at conferences such as the International Seating Symposium, European Seating Symposium, and World Federation of OT Congress. Eleni is an ongoing guest lecturer at New York University and was elected to Chair of the RESNA International Special Interest Group (SIG) for the 2020-2022 term.