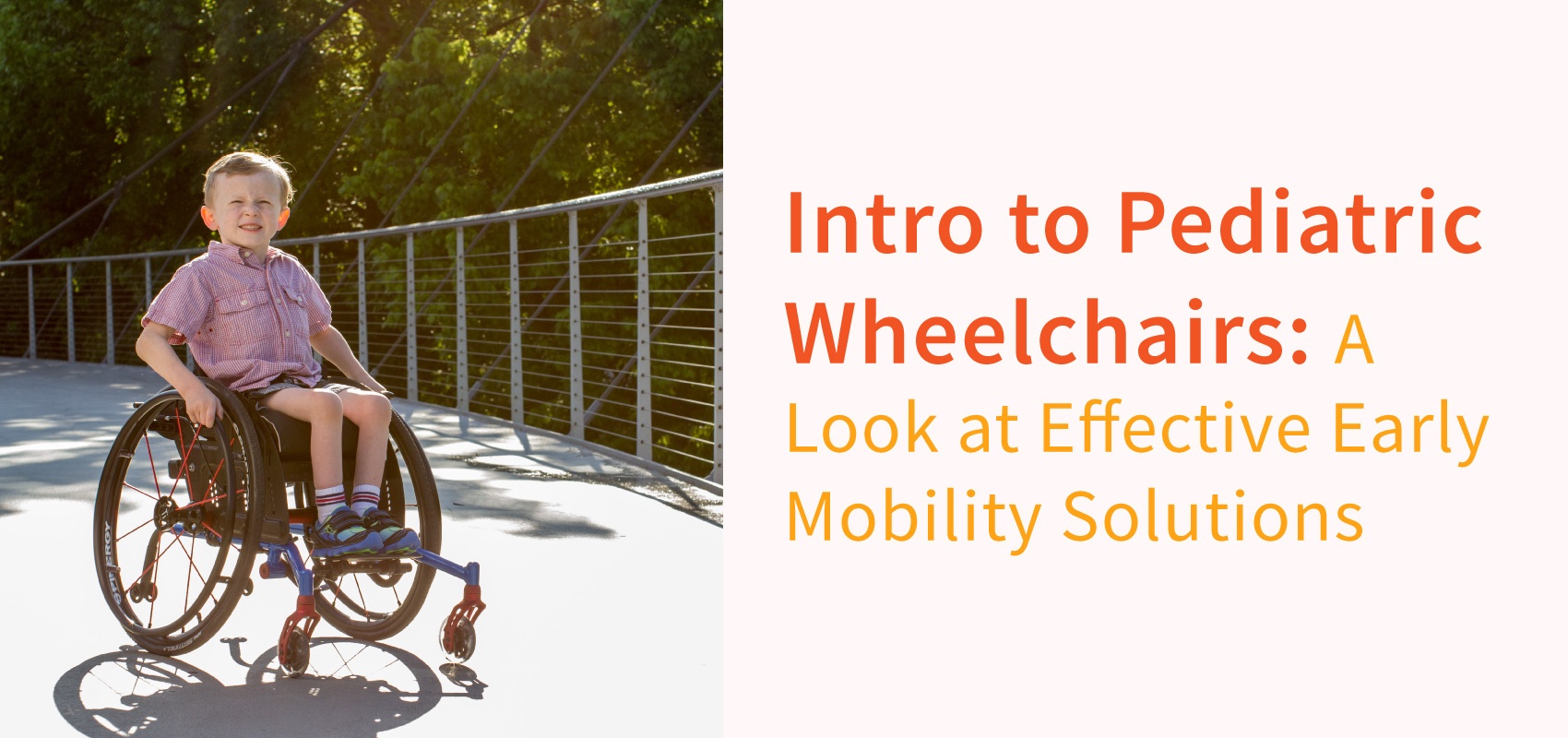
As parents, our mission is to provide our children with what they need to thrive and develop into their best selves. When my kids were babies, I was amazed by how quickly they went from being completely dependent in the first weeks, to being able to roll over, hold their head up, and reach for toys within a few months. I blinked and all of a sudden they were running circles around me! Children need to move as it plays a large part in their motor, sensory, emotional, and social development.
By 7-9 months a child typically begins to crawl and gain freedom to explore his/her environment, putting parents on high alert. When a child reaches 10-12 months they can typically stand independently and even take a few steps (3). They can move in and out of various positions to explore their environment and satisfy their curiosities. This ability to move is shaping neural pathways and developing various sensory and motor systems: visual motor skills, depth perception, position in space, socialization, cause and effect, to name a few.
So, what happens when a child has a condition that limits their ability to move independently?
Because early mobility is so critical to development, there has been a focus in pediatric rehabilitation on effective early mobility (1). It used to be that therapists would be more focused on stages of development, and mobility would be addressed only when other developmental skills had been achieved. Not anymore! Therapists now recognize the importance of independent movement and the effect it can have on childhood development.
What is effective early mobility?
Effective mobility refers to how functional it is for daily tasks. For example, a child with cerebral palsy may be able to walk 20ft with minimal assistance, but is this effective and efficient mobility to navigate the hallways of a large school? Probably not. This is why pediatric therapists will work on ambulation, but they will also facilitate and instruct in more effective means of mobility. This doesn’t mean that that child stops walking the 20ft with minimal assistance! It means that perhaps he walks with minimal assistance in the home but uses a mobility device outside the home to optimize effective and efficient mobility.
This is what makes the topic interesting. There isn’t one solution for everybody, and sometimes it is a combination of solutions that will work best! This series is going to address these issues and introduce you to various early mobility options for children that can allow effective mobility for daily function. The goal is to increase awareness of the importance of early mobility and empower you as parents to seek out what will be most effective and efficient for your child’s mobility needs. We believe every child has the right to thrive, grow in independence and socialization, and be their best selves!
Here’s a quick look at some of the topics our series will cover:
Common Questions and Misconceptions
- There are several common concerns that parents, therapists, and teachers have related to early mobility. We will address these concerns and clarify gray areas.
Manual mobility options: Dependent vs iIndependent
- There are various options for manual mobility that range from strollers to ultra-lightweight wheelchairs. We will walk through the options and detail how a manual chair can grow with your child.

Power Assist and Manual Mobility
- With the continued theme of effective mobility, this option can provide the extra boost needed for a child to keep up with his/her peers without going to a full power wheelchair.
Power Mobility Options
- This option is frequently misunderstood, and we will clear up misconceptions to get to the many potential benefits. New creative technology is available for young children to explore their environment that look a lot different than adult power wheelchairs.
How do I decide which will be best for my child?
- This question will be addressed throughout the series. It’s important to think of the child’s effective mobility, but parental considerations need to be thought out as well.
Join us as we tackle these topics and offer many more practical tips related to early mobility!
References:
1. Rosen, L., Plummer, T., Sabet, A., Lange, M., & Livingstone, R. (2017). RESNA Position on the Application of Power Mobility Devices for Pediatric Users-Update 2017. Retrieved from https://www.resna.org/sites/default/files/legacy/Position-Papers/RESNA%20Ped%20Power%20Paper%2010_25_17%20-BOD%20approval%20Nov2_2017.pdf
2. Livingstone, R. (2011). Evidence for Practice- Power Mobility for School-Aged Children and Adolescents[Ebook]. Vancouver, British Columbia: Sunny Hill Health Centre for Children.
3. Milestones Checklist. (2018). Retrieved from https://pathways.org/wp-content/uploads/2015/06/MilestonesChecklist_UPDATED.pdf

Stacey Mullis, OTR/ATP
Director of Clinical Marketing
Stacey is Director of Clinical Marketing. She graduated from Western University in London, Ontario, Canada with a BA Linguistics and BSc Occupational Therapy and has practiced as an OTR for over 20 years. With experience in pediatrics, inpatient/outpatient rehabilitation, long term care, and home health, Stacey has faced the challenges first hand of providing appropriate seating in various clinical settings. This led her to pursue an apprenticeship at Care Partners Seating Clinic in Asheville, NC to advance her skills, and she obtained her ATP certification in 2012. Mullis is a member of the NCOTA, CTF, NRRTs, RESNA, and AOTA.