Part 4 in our series on Dementia. Check out Part 1, Part 2, and Part 3.
When talking to the loved one of a resident with dementia, statements are often made such as: 
In my opinion, the most devastating loss when dealing with dementia is we are looking at the shell of the person and the personality we know and love is no longer with us. They now curse, yell, or scream when they used to be so gentle and kindly mannered. Or maybe they have softened and they are no longer the feisty being we once knew. Whatever the case may be, treatment is difficult for someone whose temperament is so radically different, and we just never know what to expect. This uncertainty can pose an issue for treatment.
Common temperament changes include:
- Inappropriate behavior
- Personality changes
- Emotional instability
- Aggressive behavior
- Mood swings
- Anxiety
- Depression
- Anger
- Stress
With the temperamental changes that result from dementia, we have to understand that a resident may be less trusting and unsure of the tiniest change made to their wheelchair system.
Here are some best practices I've found to be successful in my treatment approach:
-
Educate the family and staff extensively on the need for and type of change to the wheelchair system so they can be on board and help you make the change with the resident.
-
Take the “backseat” when approaching the resident and let the familiar face of the family or staff member make the change. Act as though you are simply a bystander there to assist.
-
Suggest to the family that they present a change as the “new Cadillac model” to create that “new car feeling.” Who doesn’t love a new car, right?
-
Sometimes the less-is-more approach is best. Don’t give hefty explanations to the resident that will overwhelm and confuse them. Using too many words can throw the resident into a spiral of irrational behavior. Some families choose to change out the wheelchair when the resident isn’t aware. They wait and see if issues arise in the form of verbal complaints or increase in unwanted behaviors, which is a common sign of pain or discomfort in a resident with dementia. If no negative behaviors appear, it is safe to assume that the change is A-Okay.
-
Make one change at a time and give the resident sufficient time to adapt to the change. Remember, studies suggest it takes two to three weeks with someone with dementia to acclimate to a change in routine. We want to avoid overwhelming his or her system at all cost.
Another issue to consider is that a resident with dementia often times presents with anxiety, aggression, uncontrolled stress, irritability, and mood swings. This type of resident is more inclined to wiggle, fidget, and continuously attempt to get up unassisted from the chair. This places them at risk to fall from the chair and may increase susceptibility to injury and wound development. We HAVE TO consider that an ill-fitting wheelchair could increase this behavior. They may perceive the chair as uncomfortable and/or painful, causing them to sit in abnormal postures.
Attempt to make the wheelchair “fit like a glove” by capturing his/her individual shape. This will make the resident feel safe and comfortable in the wheelchair system. It will decrease falls, prevent wounds, and decrease the unwanted behavioral changes that would arise from sitting in an ill-fitting chair.
Your goal with this type of resident should be to:
-
Look for a model of wheelchair that can be adjusted to the resident’s exact dimensions. And, trust me, the overused K0001 and K0002 chairs commonly seen in the nursing home won’t do the trick. I suggest a K0004 model.
-
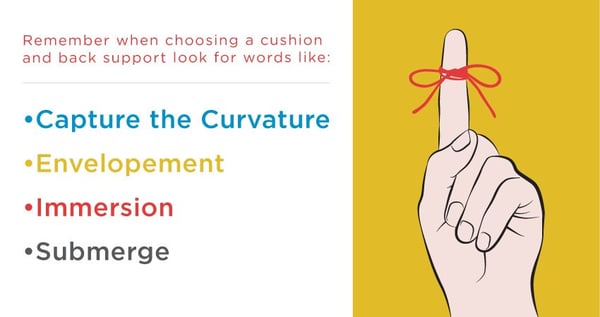
Look for cushions that immerse the pelvis and alleviate pressure and that may have contours to assist with proper pelvic and LE alignment.
-
Don’t stop at the cushion! Replace the sling back that comes on all chairs. Taut back upholstery that comes on a chair may make a resident feel “pushed out” of the chair. That tactile cue will increase attempts to get up out of the chair. That is the LAST thing we want for the resident–to get up unassisted!
-
Look for a back support that gives you the opportunity to envelop the spine and capture the curvature of the resident. This will decrease pain and relieve peak pressures.
See you next week when we explore sensation issues as a result of the damage to the brain in residents with dementia.

Ana Endsjo, MOTR/L, CLT
Clinical Education Manager LTC Division
Ana Endsjo has worked as an occupational therapist since 2001 in a variety of treatment settings. She has mainly worked with the geriatric population, dedicated to the betterment of the treatment of the elderly in LTC centers. Her focus has been on seating and positioning and contracture management of the nursing home resident. With this experience, her hope is to guide other therapists, rehab directors, nurses, and administrators through educational guides, blogs, webinars, and live courses in her role as Clinical Education Manager for the long term care division.

